NICE - decompressive hemicraniectomy for ischaemic stroke
Decompressive hemicraniectomy in ischaemic stroke
- ischaemic stroke is one of the leading causes for death and disability worldwide
- in patients with large space-occupying infarction, the subsequent oedema complicated by transtentorial herniation poses a lethal threat
- this occurs particularly in patients with malignant middle cerebral artery infarction, brain swelling secondary to the vessel occlusion is associated with high mortality
- patients with large hemispheric infarction may suffer from increasing intracranial pressure (ICP) resulting in cerebral herniation and subsequent mechanical and ischemic damage of healthy cerebral territories (1)
- in 1-10% of all patients with acute middle cerebral artery occlusion, the subsequent ischemic stroke can be classified as "malignant," defined by ischemic brain tissue large enough to cause considerable increase of ICP and potential cerebral herniation (2)
- decompressive craniectomy in this scenario
- a significant proportion of the skull is surgically removed, allowing the ischaemic tissue to shift through the surgical defect rather than to the unaffected regions of the brain, thus avoiding secondary damage due to increased intracranial pressure
- study evidence has shown that decompressive craniectomy reduces the mortality rate in patients with malignant cerebral artery infarction (3)
- however, this is done for the cost of a higher proportion of patients who survive with severe disability.
- this occurs particularly in patients with malignant middle cerebral artery infarction, brain swelling secondary to the vessel occlusion is associated with high mortality
- in patients with large space-occupying infarction, the subsequent oedema complicated by transtentorial herniation poses a lethal threat
NICE suggest that a decompressive hemicraniectomy (which should be performed within 48 hours of symptom onset) should be considered for people with acute stroke who meet all of the following criteria:
- clinical deficits that suggest infarction in the territory of the middle cerebral artery, with a score above 15 on the NIHSS
- decreased level of consciousness, with a score of 1 or more on item 1a of the NIHSS
- signs on CT of an infarct of at least 50% of the middle cerebral artery territory:
- with or without additional infarction in the territory of the anterior or posterior cerebral artery
- on the same side or with infarct volume greater than 145 cm3, as shown on diffusion-weighted MRI scan
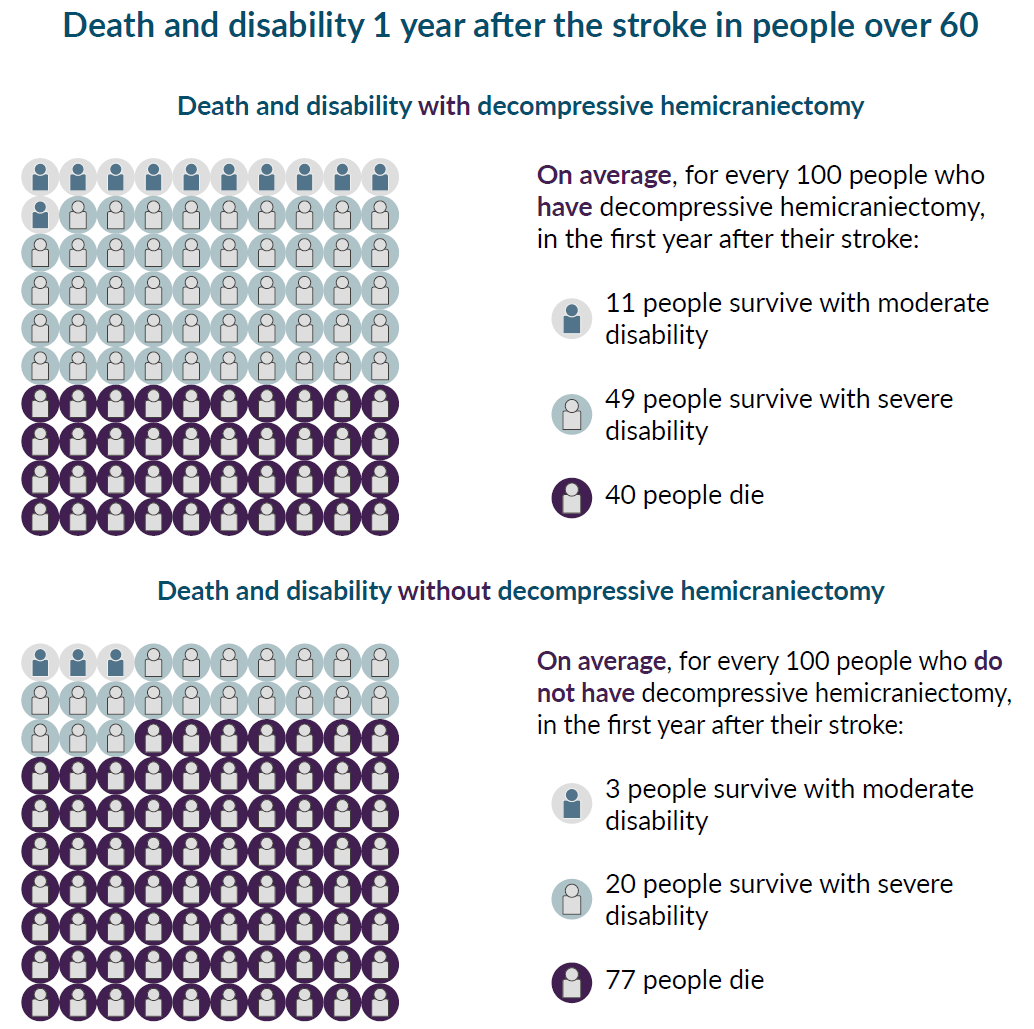
NICE have suggested estimates of risk and harm of decompressive hemicraniectomy in people with a stroke either under or over 60 years of age:

Reference:
- Stokum JA, Gerzanich V, Simard JM. Molecular pathophysiology of cerebral edema. J Cereb Blood Flow Metab. (2016) 36:513-38
- Hacke W et al. 'Malignant' middle cerebral artery territory infarction: clinical course and prognostic signs. Arch Neurol. (1996) 53:309-15.
- Alexander P et al. Hemicraniectomy versus medical treatment with large MCA infarct: a review and meta-analysis. BMJ Open (2016) 6:e014390. doi: 10.1136/bmjopen-2016-014390
- NICE (May 2019).Stroke and transient ischaemic attack in over 16s: diagnosis and initial management
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.