LDL and cardiovascular (CV) risk
- a 1% decrease in LDL-C is associated with a 1% decrease in CHD risk (1)
- this compares with the association that a 1% increase in HDL-C is associated with a 2-3% decrease in CHD risk
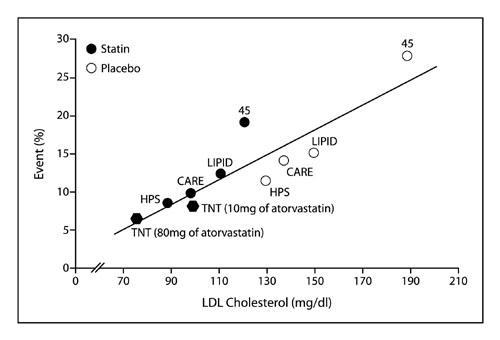
Relationship between LDL and event risk in trial data - there seems a linear reduction in risk with lowering LDL
Notes:
- clinical trial data suggest that acquired relative CV risk reduction per unit LDL-c reduction is consistent, regardless of baseline LDL-c (2)
- patients with higher baseline LDL-c though benefit most from LDL-c lowering therapy with a larger absolute LDL-c lowering and greatest reduction in mortality (3)
- a meta-analysis concluded that statin therapy can safely reduce the 5-year incidence of major coronary events, coronary revascularisation, and stroke by about one fifth per mmol/L reduction in LDL cholesterol, largely irrespective of the initial lipid profile or other presenting characteristics (4)
- in the real-world patients in the SWEDEHEART registry, early LDL-c reduction after an MI was associated with lower incidence and reduced adjusted risk of MACE, all-cause mortality, CV mortality, MI, ischemic stroke, hospitalization for HF and coronary revascularization (5)
- every 1 mmol/L reduction in LDL-c was an approximate 25% relative event rate reduction for major vascular events. Similar results were obtained for outcomes of MACE, all-cause mortality, MI and a larger reduction in event rate for hospitalization for heart failure
Reference:
- Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Programme (NCEP) Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults Adult Treatment Panel III). JAMA2001;285:2486-97.
- Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, Kirby A, Sourjina T, Peto R, Collins R, Simes R, Cholesterol Treatment Trialists' (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective LDL-C reduction and statin intensity in MI patients meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet Lond Engl 2005;366:1267-1278.
- Navarese EP, Robinson JG, Kowalewski M, Kolodziejczak M, Andreotti F, Bliden K, Tantry U, Kubica J, Raggi P, Gurbel PA. Association between baseline LDL-C level and total and cardiovascular mortality after LDL-C lowering: a systematic review and meta-analysis. JAMA 2018;319:1566-1579
- Baigent C et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005 Oct 8;366(9493):1267-78
- Schubert J, Lindahl B, Melhus H et al. Low-density lipoprotein cholesterol reduction and statin intensity in myocardial infarction patients and major adverse outcomes: a Swedish nationwide cohort study. Eur Heart J 2021, 42:243-252, doi:10.1093/eurheartj/ehaa1011
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.