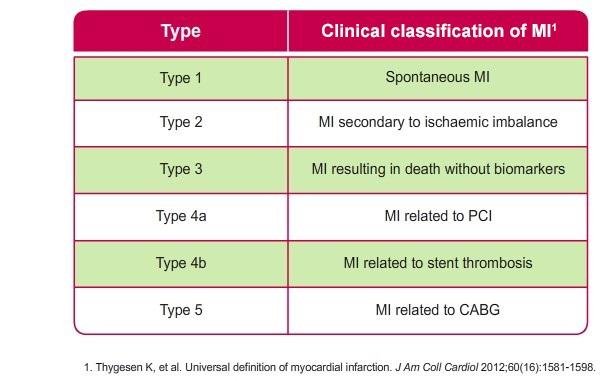
Type 1 - Spontaneous myocardial infarction (MI)
Type 1: Spontaneous myocardial infarction
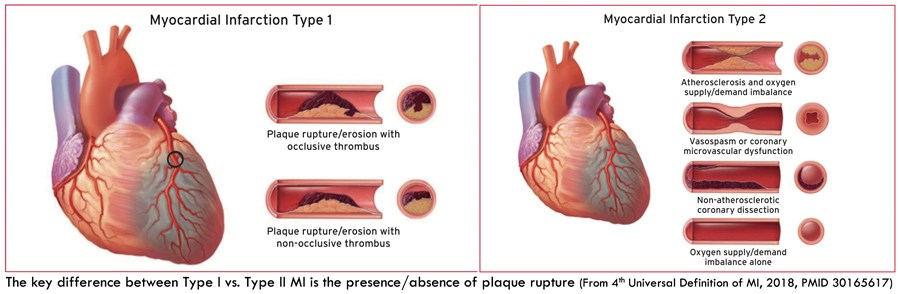
- spontaneous myocardial infarction related to atherosclerotic plaque rupture, ulceration, fissuring, erosion, or dissection with resulting intraluminal thrombus in one or more of the coronary arteries leading to decreased myocardial blood flow or distal platelet emboli with ensuing myocyte necrosis. The patient may have underlying severe CAD but on occasion non-obstructive or no CAD.
Type 2: Myocardial infarction secondary to an ischaemic imbalance
- in instances of myocardial injury with necrosis where a condition other than CAD contributes to an imbalance between myocardial oxygen supply and/or demand, e.g. coronary endothelial dysfunction, coronary artery spasm, coronary embolism, tachy-/brady-arrhythmias, anaemia, respiratory failure, hypotension, and hypertension with or without LVH.
Type 3: Myocardial infarction resulting in death when biomarker values are unavailable
- cardiac death with symptoms suggestive of myocardial ischaemia and presumed new ischaemic ECG changes or new LBBB, but death occurring before blood samples could be obtained, before cardiac biomarker could rise, or in rare cases cardiac biomarkers were not collected.
Type 4a: Myocardial infarction related to percutaneous coronary intervention (PCI)
- myocardial infarction associated with percutaneous coronary intervention is arbitrarily defined by elevation of cardiac troponin values >5 x 99th percentile URL in patients with normal baseline values (<=99th percentile URL) or a rise of cardiac troponin values >20% if the baseline values are elevated and are stable or falling. In addition, either (i) symptoms suggestive of myocardial ischemia, or (ii) new ischemic electrocardiographic changes or new left bundle branch block, or (iii) angiographic loss of patency of a major coronary artery or a side branch or persistent slow-flow or no-flow or embolization, or (iv) imaging demonstration of new loss of viable myocardium or new regional wall motion abnormality are required.
Type 4b: Myocardial infarction related to stent thrombosis
- myocardial infarction associated with stent thrombosis is detected by coronary angiography or autopsy in the setting of myocardial ischaemia and with a rise and/ or fall of cardiac biomarkers values with at least one value above the 99th percentile URL
Type 5: Myocardial infarction related to coronary artery bypass grafting (CABG)
- myocardial infarction associated with CABG is arbitrarily defined by elevation of cardiac biomarker values >10 x 99th percentile URL in patients with normal baseline cTn values (<=99th percentile URL). In addition, either (i) new pathological Q waves or new LBBB, or (ii) angiographic documented new graft or new native coronary artery occlusion, or (iii) imaging evidence of new loss of viable myocardium or new regional wall motion abnormality.
The universal definition differentiates patients with:
- myocardial infarction due to plaque rupture (type 1) from
- those due to myocardial oxygen supply-demand imbalance (type 2) secondary to other acute illnesses
- patients with myocardial necrosis, but no symptoms or signs of myocardial ischaemia, are classified as acute or chronic myocardial injury
- this classification has not been widely adopted in practice, because the diagnostic criteria for type 2 myocardial infarction encompass a wide range of presentations, and the implications of the diagnosis are uncertain. However, both myocardial injury and type 2 myocardial infarction are common, occurring in more than one-third of all hospitalised patients. These patients have poor short-term and long-term outcomes with two-thirds dead in 5 years (1).
The third universal definition of myocardial infarction provided an international consensus on the classification of myocardial injury and infarction (2):
- the diagnosis of myocardial infarction requires evidence of myocardial necrosis in a clinical setting consistent with acute myocardial ischaemia. These criteria require detection of a rise and/or fall in cardiac biomarker levels (preferably cardiac troponin) with at least one value above the 99th percentile upper reference limit, with at least one of the following:
- (1) symptoms of myocardial ischaemia,
- (2) new or presumed new significant ST-segment T-wave changes or new left bundle branch block,
- (3) development of pathological Q-waves on the electrocardiogram,
- (4) imaging evidence of loss of viable myocardium or new regional wall motion abnormality or
- (5) identification of intracoronary thrombus by angiography or autopsy
The classification (2) distinguishes between type 1 myocardial infarction due to thrombosis of an atherosclerotic plaque and type 2 myocardial infarction due to myocardial oxygen supply demand imbalance in the context of another acute illness
- myocardial infarctions presenting as sudden death (type 3), or
- after percutaneous coronary intervention (type 4) and
- coronary artery bypass grafting (type 5) are also defined
- differentiating between patients with type 2 myocardial infarction and those patients with myocardial necrosis in the absence of ischaemia, in whom the recommended classification is myocardial injury, is challenging, as there is considerable overlap between these two clinical entities
Acute myocardial injury is classified where troponin concentrations are elevated with evidence of dynamic change in the absence of overt myocardial ischaemia, whereas in chronic myocardial injury troponin concentrations remain unchanged on serial testing
- an important distinction, as the underlying pathological mechanisms in acute and chronic myocardial injury are likely to differ
- classification is contentious and was based on expert consensus rather than evidence from prospective clinical trials (1)
Reference:
- Chapman AR et al. Assessment and classification of patients with myocardial injury and infarction in clinical practice.Heart 2017;103:10-18
- Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Eur Heart J 2012;33:2551-67.
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.