Management
Diagnosis:
- lesions can be swabbed and samples sent for culture
- NICE (1) do not suggest mandatory initial swabbing of lesions but note:
- if a skin swab has been sent for microbiological testing:
- review the choice of antibiotic when results are available and
- change the antibiotic according to results if symptoms are not improving, using a narrow-spectrum antibiotic if possible
- if a skin swab has been sent for microbiological testing:
Topical treatment:
- topical fusidic acid or mupirocin
- there is evidence that topical antibiotics may be slightly more effective than oral antibiotics for patients with limited non-bullous impetigo (2). Disinfecting treatments are not effective (2)
- topical antibiotic therapy is indicated in localized cases without complications (3)
- topical mupirocin is a very effective treatment option
- topical fusidic acid cream an effective treatment for impetigo with very few side-effects, equally effective, in fact, as mupirocin.
Systemic treatment - if widespread
- systemic antimicrobials are the treatment of choice for widespread infections and infections complicated by systemic symptoms (3)
- recommended oral antibiotic choices are flucloxacillin or erythromycin, or a cephalosporin such as cefalexin or cefradine (4)
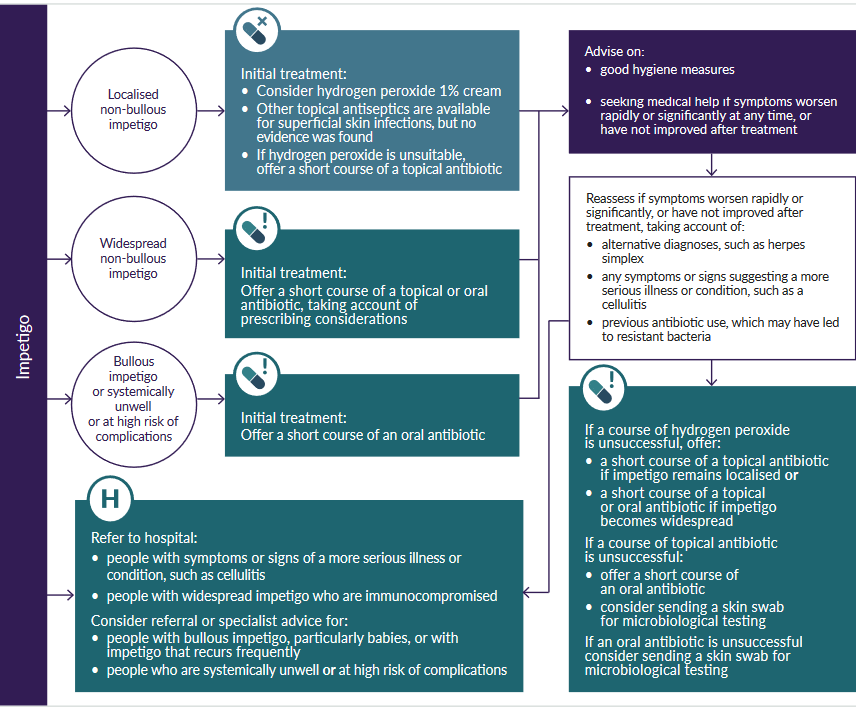
NICE suggest an algorithm for treatment based on features of the impetigo presenting to the clinician (1):
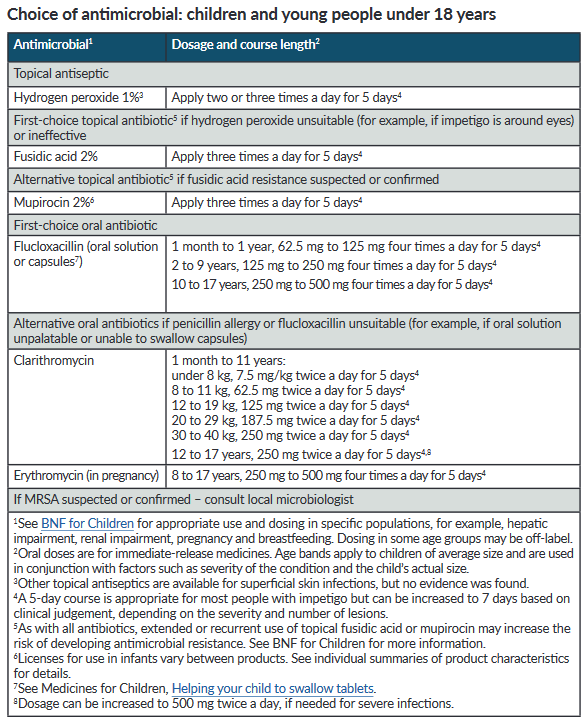
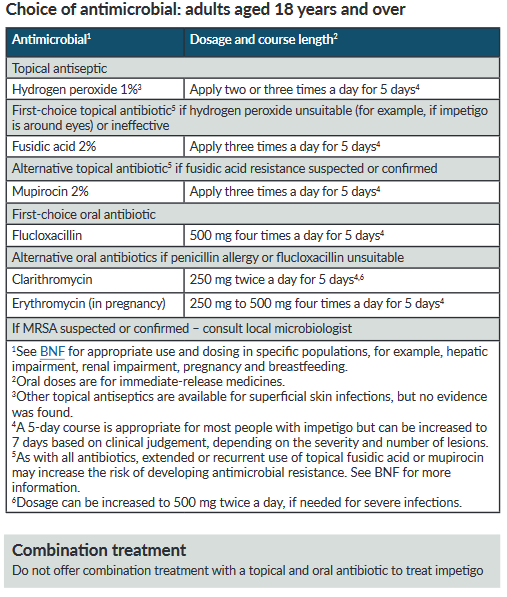
Antibiotic treatments have been suggested by NICE (1):
Patient eduction:
- good handwashing techniques
- avoid scratching - cutting finger-nails may be useful
Notes:
- previously been stated that topical treatment for 7 days is generally adequate for limited disease - the maximum duration of topical treatment is 10 days (4)
- if using systemic treatment and streptococcal infection is suspected then add phenoxymethylpenicillin to flucloxacillin (co-amoxiclav is an alternative to using phenoxymethylpenicillin and flucloxacillin together)
Reference:
- NICE (February 2020).Impetigo: antimicrobial prescribing
- Koning S etl al (2004). Interventions for impetigo. Cochrane Database Syst Rev 2004; (2)CD003261.
- Brown J et al. Impetigo: an update. Int J Dermatol. 2003 Apr;42(4):251-5
- Prescriber (2004); 15 (13): 35-40.
- Public Health England (June 2021). Managing common infections: guidance for primary care
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.