Vulvar and vaginal atrophy
Genitourinary syndrome of menopause (GSM; previously known as vulvovaginal atrophy or atrophic vaginitis) involves symptoms of vaginal dryness, burning, and itching as well as dyspareunia, dysuria, urinary urgency, and recurrent urinary tract infections (1):
- is estimated that nearly 60% of women in menopause experience GSM but the majority of these women do not bring up this concern with their health care provider
- studies also show that only 7% of health care providers ask women about this condition
- GSM means clinically is that the vaginal and vulvar tissue becomes thin and dry, which often leads to a burning sensation, itching, and pain and dryness during sex
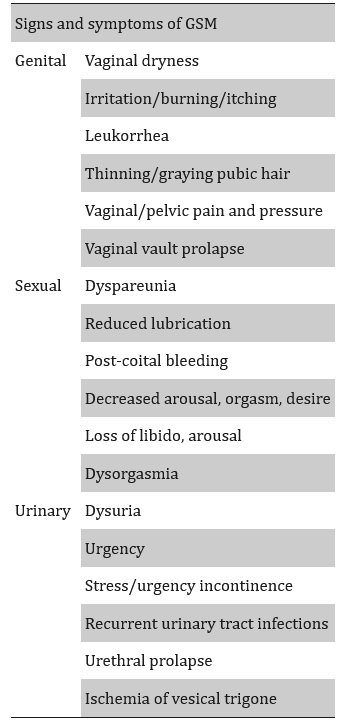
GSM is a chronic, progressive, vulvovaginal, sexual, and lower urinary tract condition characterized by a broad spectrum of signs and symptoms (2)
- most of these symptoms can be attributed to the lack of oestrogen that characterizes menopause
- even though the condition mainly affects postmenopausal women, it is seen in many premenopausal women as well
Vaginal resistance to infection and injury is reduced in the postmenopausal woman through lack of oestrogen which causes:
- thinning of the vulval and vaginal epithelium
- loss of glycogen
- fall in acidity
- absence of protective lactobacilli
Symptoms of GSM (2)
Differential diagnosis in possible GSM:
- clinicians should always exclude other causes with similar symptoms and, specifically, dermatological conditions of the vulva such as lichen sclerosus or planus, eczema, dermatitis, chronic vulvovaginitis, vaginitis and vaginosis, vulvodynia, malignancies, and chronic pelvic pain (2)
Diagnosis of GSM in primary care (3):
- based on a history of typical symptoms that may be accompanied by signs on examination
- clinicians should take note of pre-existing skin conditions, vulval skin products, previous birth trauma, and/or prolapse that may contribute to symptoms and make alternative diagnoses more likely
- examination
- findings in early disease can be subtle and difficult to detect
- can include a pale and thinned appearance of the vulva and vagina, with friable tissue
- vagina may be shortened or narrowed, with loss of rugae
- may be decreased secretions or a watery discharge
- findings in later disease
- labia may be reduced in size or fused, and the clitoris may be concealed or more prominent
- findings in early disease can be subtle and difficult to detect
- re-examination is required for persistent symptoms despite treatment and for patients whose symptoms change or deteriorate
If urinary frequency as a presenting symptom
- exclude UTI and diabetes
- noted that (3):
- a discussion regarding reducing consumption of bladder irritants, treating concurrent constipation, and filling out a bladder diary may also be helpful
- stress and urge incontinence can be multifactorial, and while providing vaginal oestrogen may help with severity, underlying causes such as prolapse, weak pelvic floor muscles, and overactive bladder should be addressed simultaneously
If blood-stained discharge then consider as postmenopausal bleeding - manage in context of NICE guidance (linked item).
If vaginal discharge in woman aged 55 or over - manage in context of NICE guidance (linked item).
Other investigations to consider will depend on presenting clinical features:
- swabs
- if vaginal discharge then an infection screen may be appropriate > to exclude vaginal infections or endometritis
- pelvic scans
- for example, when patients report associated pelvic pain or pressure symptoms
- where there is uncertainty about the diagnosis, further advice should be sought from vulval dermatology, gynaecology, urology, or sexual health depending on primary presentation
Management principles:
- moisturisers, lubricants, and local oestrogen preparations are cheap, safe, and effective treatments
- local (vaginal) oestrogen has been shown to improve vaginal dryness dysuria, frequency, urge, and stress incontinence, and reduce recurrent UTIs in menopausal patients (3)
- general advice on vulval hygiene should be provided and patients should be advised to avoid wet wipes, perfumed soaps, and douching (3)
- ospemifene is the only oral treatment available that may support increased treatment satisfaction and adherence (3)
Notes:
- consider screen for diabetes (uncontrolled diabetes can contribute to symptoms)
Reference:
- Peters KJ. What Is Genitourinary Syndrome of Menopause and Why Should We Care? Perm J. 2021 May;25:20.248.
- Angelou K, Grigoriadis T, Diakosavvas M, Zacharakis D, Athanasiou S. The Genitourinary Syndrome of Menopause: An Overview of the Recent Data. Cureus. 2020 Apr 8;12(4):e7586.
- Burgin J et al. Genitourinary syndrome of menopause. BJGP 2025; 75 (761): 583-585.
Related pages
- Treatment of atrophic vaginitis
- Postmenopausal bleeding - NICE urgent cancer referral guidance
- Vaginal discharge (unexplained) either at first presentation or with thrombocytosis or with haematuria, in women 55 and over - urgent cancer referral guidance
- Vulval bleeding - NICE urgent cancer referral guidance
- Assessment of vaginal discharge
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.