Familial breast cancer
Up to 10% of breast cancer in Western countries is due to genetic predisposition. Susceptibility to breast cancer appears to be inherited as an autosomal dominant with limited penetrance and may thus be inherited from either the father or mother. About 5% of breast cancer is due to highly penetrant dominant genes.
More than five genes are thought to be involved. The most important appears to be the BRCA1 gene located on chromosome 17q. This has recently been cloned and thought to have mutations present at different regions. Other genes identified include BRCA2 on 13q and the p53 gene on 17p.
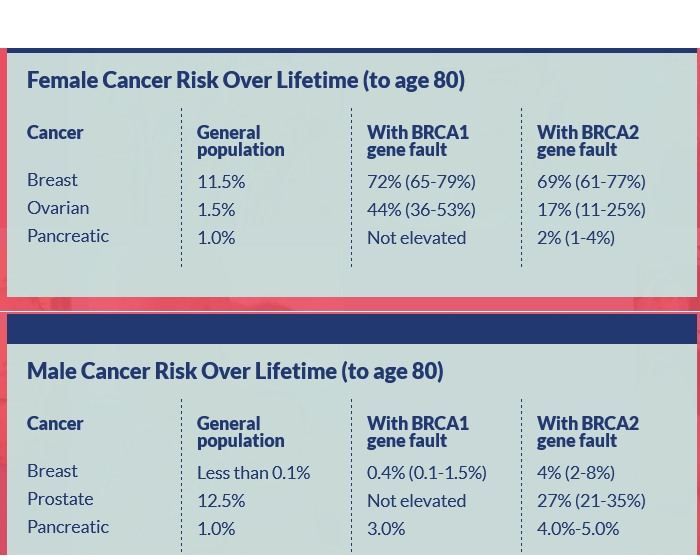
- BRCA1 carriers have a lifetime risk approaching 80% of developing breast cancer and an increased risk of ovarian cancer (40-60%) (1)
- BRCA2 confers a lower risk of ovarian cancer (20-30%) but is associated with an increased risk of a wider spectrum of other cancers including prostate cancer, pancreatic cancer, and an increased risk of male breast cancer
- in the UK general caucasian population - the frequency of mutations in BRCA1 or BRCA2 is approximately 1/400; in the Ashkenazim population the frequency of these mutations is about 2% (1)
- management of breast cancers in BRCA1 and BRCA2 carriers is currently the same as for sporadic cases, except that bilateral mastectomy may be offered at the time of primary surgery because of the increased risk of development of breast cancer in the contralateral breast (about 4% per year) (1)
Characteristics of familial breast cancer include:
- early age of presentation
- several relatives are affected
- bilateral involvement is common
- history of related cancers - colorectal, ovary, endometrium
If a first-degree relative has breast carcinoma, the relative risk of developing breast carcinoma is 1.7 to 2.5. If a second-degree relative is affected, the relative risk is 1.5.
DNA tests are possible for a few suitable families.
Mutations in the CHEK2 gene may increase the risk of breast cancer two-fold (1).
Mutations in the TP53 gene increase the risk of a wide spectrum of tumours, including sarcomas, adrenocortical carcinomas, brain cancer, and very early-onset breast cancer.
NICE suggest (4):
- Carrier probability at which genetic testing should be offered
- When available in secondary care, use a carrier probability calculation method with demonstrated acceptable performance (in calibration and discrimination), as well as family history, to determine who should be offered referral to a specialist genetic clinic. Examples of acceptable methods include BOADICEA and the Manchester scoring system
- offer genetic testing in specialist genetic clinics to a relative with a personal history of breast and/or ovarian cancer if that relative has a combined BRCA1 and BRCA2 mutation carrier probability of 10% or more
- offer genetic testing in specialist genetic clinics to a person with no personal history of breast or ovarian cancer if their combined BRCA1 and BRCA2 mutation carrier probability is 10% or more and an affected relative is unavailable for testing
- Breast cancer risk category
Near population risk | Moderate risk | High Risk * | |
Lifetime risk from age 20 | Less than 17% | Greater than 17% but less than 30% | 30% or greater |
Risk between ages 40 and 50 | Less than 3% | 3-8% | Greater than 8% |
*This group includes known BRCA1, BRCA2 and TP53 mutations and rare conditions that carry an increased risk of breast cancer such as Peutz-Jegher syndrome (STK11), Cowden (PTEN) and familial diffuse gastric cancer (E-Cadherin)
- Surveillance for women with no personal history of breast cancer
- Offer annual mammographic surveillance to women:
- aged 40-49 years at moderate risk of breast cancer
- aged 40-59 years at high risk of breast cancer but with a 30% or lower probability of being a BRCA or TP53 carrier
- aged 40-59 years who have not had genetic testing but have a greater than 30% probability of being a BRCA carrier
- aged 40-69 years with a known BRCA1 or BRCA2 mutation
- Offer annual MRI surveillance to women:
- aged 30-49 years who have not had genetic testing but have a greater than 30% probability of being a BRCA carrier
- aged 30-49 years with a known BRCA1 or BRCA2 mutation
- aged 20-49 years who have not had genetic testing but have a greater than 30% probability of being a TP53 carrier
- aged 20-49 years with a known TP53 mutation
- Offer annual mammographic surveillance to women:
- Surveillance for women with a personal and family history of breast cancer
- offer annual mammographic surveillance to all women aged 50-69 years with a personal history of breast cancer who:
- remain at high risk of breast cancer (including those who have a BRCA1 or BRCA2 mutation), and
- do not have a TP53 mutation
- offer annual MRI surveillance to all women aged 30-49 years with a personal history of breast cancer who remain at high risk of breast cancer, including those who have a BRCA1 or BRCA2 mutation
- offer annual mammographic surveillance to all women aged 50-69 years with a personal history of breast cancer who:
- Chemoprevention for women with no personal history of breast cancer
- offer either tamoxifen or raloxifene for 5 years to postmenopausal women with a uterus and at high risk of breast cancer unless they have a past history or may be at increased risk of thromboembolic disease or endometrial cancer
- offer either tamoxifen or raloxifene for 5 years to postmenopausal women with a uterus and at high risk of breast cancer unless they have a past history or may be at increased risk of thromboembolic disease or endometrial cancer
- Risk-reducing mastectomy for women with no personal history of breast cancer
- all women considering bilateral risk-reducing mastectomy should be able to discuss their breast reconstruction options (immediate and delayed) with a member of a surgical team with specialist oncoplastic or breast reconstructive skills
Breast cancer risk if family history of breast cancer
- UK modelling study found cumulative breast cancer risk for those with an ‘average’ family history taking no HRT is 9.8%, increased to 11.0% with 5 years’ combined cyclical HRT. For those with a strong family history, the risk is 19.6% (no HRT), increasing to 22.4% for 5 years’ HRT (5)
- for example, for an ‘average’ 51-year-old on combined HRT for 5 years, the likelihood of developing breast cancer attributable to HRT is 1 in 67
- for those with a strong family history, the respective likelihood is 1 in 30
- the authors conclude that although those with a significant (‘strong’) family history of breast cancer have a substantially increased baseline risk of developing breast cancer, most of the breast cancer incidence and mortality for this group will be attributable to their baseline risk rather than from the addition of HRT taken at age 50
- for example, for an ‘average’ 51-year-old on combined HRT for 5 years, the likelihood of developing breast cancer attributable to HRT is 1 in 67
The NHS Jewish BRCA Testing Programme state the various cancers associated with BRCA1 and BRACA2:
Reference:
- Pulse (2005); 65(14):55-60.
- Evans DGR et al. (1994). Familial breast cancer. BMJ; 308:183-7
- McPherson et al. (1994). BMJ;309: 1004
- NICE (June 2013). Familial breast cancer - Classification and care of people at risk of familial breast cancer and management of breast cancer and related risks in people with a family history of breast cancer
- Huntley C et al. Breast cancer risk assessment for prescription of Menopausal Hormone Therapy in women who have a family history of breast cancer. British Journal of General Practice 9 May 2024
Related pages
- Breast cancer
- Prophylactic mastectomy in patients with BRCA mutations
- Risk of ovarian cancer with respect to family history
- Referral criteria from primary care - if family history of breast cancer
- TP53 gene
- Chemoprevention if no personal history of breast cancer
- Mastectomy if no personal history of breast cancer
- Oophorectomy if no personal history of breast cancer
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.