This podcast episode is worth 0.3 CPD credits. Upgrade to Pro
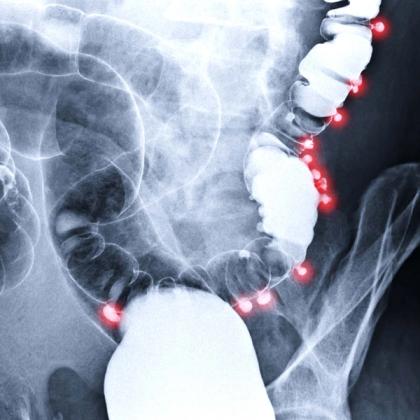
Diverticular disease is a condition characterised by the presence of small pouches, called diverticula, in the wall of the colon (large intestine). These pouches can develop when weak spots in the colon's muscular wall give way under pressure. Diverticular disease encompasses two main conditions: diverticulosis and diverticulitis. In this episode, Dr Roger Henderson takes an overview look at the symptoms and management of these as well as their prognosis and prevention.
Key references
- Stollman N and Raskin JB. Lancet. 2004;363(9409):631-9. doi: 10.1016/S0140-6736(04)15597-9.
- Tursi A. J Gastrointestin Liver Dis. 2019;28:225-235. doi: 10.15403/jgld-184.
- NICE. Guideline. Diverticular disease: diagnosis and management (NG147). 27 November 2019.
- Sánchez-Velázquez P, et al. Eur J Gastroenterol Hepatol. 2016;28(6):622-7. doi: 10.1097/MEG.0000000000000610.
- Byrnes MC and Mazuski JE. Surg Infect (Larchmt). 2009;10(2):143-54. doi: 10.1089/sur.2007.087.
- Peery AF, et al. Gastroenterology. 2021;160(3):906-911.e1. doi: 10.1053/j.gastro.2020.09.059.
Key take-home points
- Diverticular disease is best defined as any clinical state caused by symptoms linked to diverticula in the large bowel. These are a herniation of mucosa through thickened colonic muscle and may be solitary or there may be hundreds present.
- Diverticulosis refers to the presence of diverticula that are asymptomatic. Diverticular disease is when diverticula cause symptoms and is sometimes also referred to as painful diverticular disease.
- Diverticulitis indicates inflammation of a diverticulum or diverticula and may be caused by infection. Other complications of diverticular disease include bleeding, infection, abscess, perforation, peritonitis, fistula formation and bowel obstruction.
- Low dietary fibre intake is thought to be the main contributing factor along with increasing age. Other causes include lack of exercise, obesity (especially in younger people), increased red meat consumption, tobacco smoking, excessive alcohol and caffeine intake, steroids and non-steroidal anti-inflammatory drugs.
- Around three quarters of people with diverticula have no symptoms. Of the rest who do develop symptoms, about three quarters of these will develop diverticulitis. The severity of acute diverticulitis is graded using the Hinchey classification.
- There are many possible other diagnoses that need to be considered when looking at a possible diagnosis of diverticular disease.
- No investigations are required in cases of asymptomatic diverticulosis. In simple diverticular disease a full blood count should be taken, and in suspected diverticulitis, inflammatory markers (such as C-reactive protein), full blood count and urea and electrolytes should be assessed.
- Asymptomatic diverticulosis requires no treatment.
- Do not give antibiotics to people with symptomatic diverticular disease.
- If the patient has uncomplicated acute diverticulitis but is otherwise systemically well, avoid prescribing antibiotics if possible – treat with simple analgesia and advise them to return if their symptoms worsen. If the patient is unwell, is immunosuppressed or has other significant comorbidities then offer oral antibiotics. A 5-day course of amoxicillin/clavulanate is the first-line choice here.
- Patients with abdominal pain, fever, or leucocytosis who are taking oral antibiotics can be treated safely at home provided no complications are present.
- Most patients with uncomplicated diverticulitis recover following medical treatment and do not require surgical intervention.
- Mesalazine, probiotics, or antibiotics should not be used to prevent recurrent diverticulitis.
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.