Treatment of post-menopausal osteoporosis
- General management includes assessment of the risk of falls and their prevention
- a balanced diet is recommended for bone health but there is no evidence that specific diets reduce fracture risk. Changes to the diet which result in an imbalance of food groups could affect overall nutrient intake and be detrimental to general health
- calcium and vitamin D supplementation
- SIGN guidance states
- calcium and vitamin D treatment either alone or in combination are not recommended for prevention of fractures among community-dwelling postmenopausal women and older men
- calcium and vitamin D treatment may be considered for frail older people, for example nursing care residents, who are at high risk of vitamin D deficiency to reduce the risk of non-vertebral fractures
- is not necessary to measure an individual’s serum vitamin D level unless there is a clinical concern of osteomalacia
- is important to ensure patients taking antiresorptive therapy have sufficient calcium and vitamin D intake, through assessment of diet and supplementation with calcium/vitamin D or vitamin D alone accordingly
- SIGN guidance states
- exercise:
- combinations of exercise types including balance training, flexibility or stretching exercises, endurance exercise and progressive strengthening exercises should be considered to reduce risk of fractures caused by falls
- static weight-bearing exercise, for example, single-leg standing should be considered to slow decline of hip BMD
- progressive resistance strength training exercise (such as weight training) should be considered to slow decline of femoral neck BMD, either alone or in combination with impact exercise training (such as jogging, walking or aerobics)
- walking, tai chi, progressive resistance strength training (such as weight training) and different combinations of exercise types should be considered to slow decline of lumbar spine BMD
- Major pharmacological interventions are the bisphosphonates, strontium ranelate, raloxifene and parathyroid hormone peptides
- all these interventions have been shown to reduce the risk of vertebral fracture when given with calcium and vitamin D supplements. Some have been shown to also reduce the risk of nonvertebral fractures, in some cases specifically at the hip (alendronate, risedronate, zoledronate)
- therapies used in the management of osteoporosis are designed to reduce the risk of fracture
- mechanism of action is either to reduce the rate of bone turnover (antiresorptives) or stimulate bone formation (anabolic therapies). Antiresorptive therapies include bisphosphonates, raloxifene, HRT and denosumab. Parathyroid hormones, such as teriparatide, have a purely anabolic or boneforming action. Strontium ranelate has evidence for a dual role as antiresorptive and some boneforming activity. Bisphosphonates vary in potency from the weakest, etidronate, to more potent oral therapies, risedronate, alendronate and ibandronate, through to the most potent, zoledronic acid
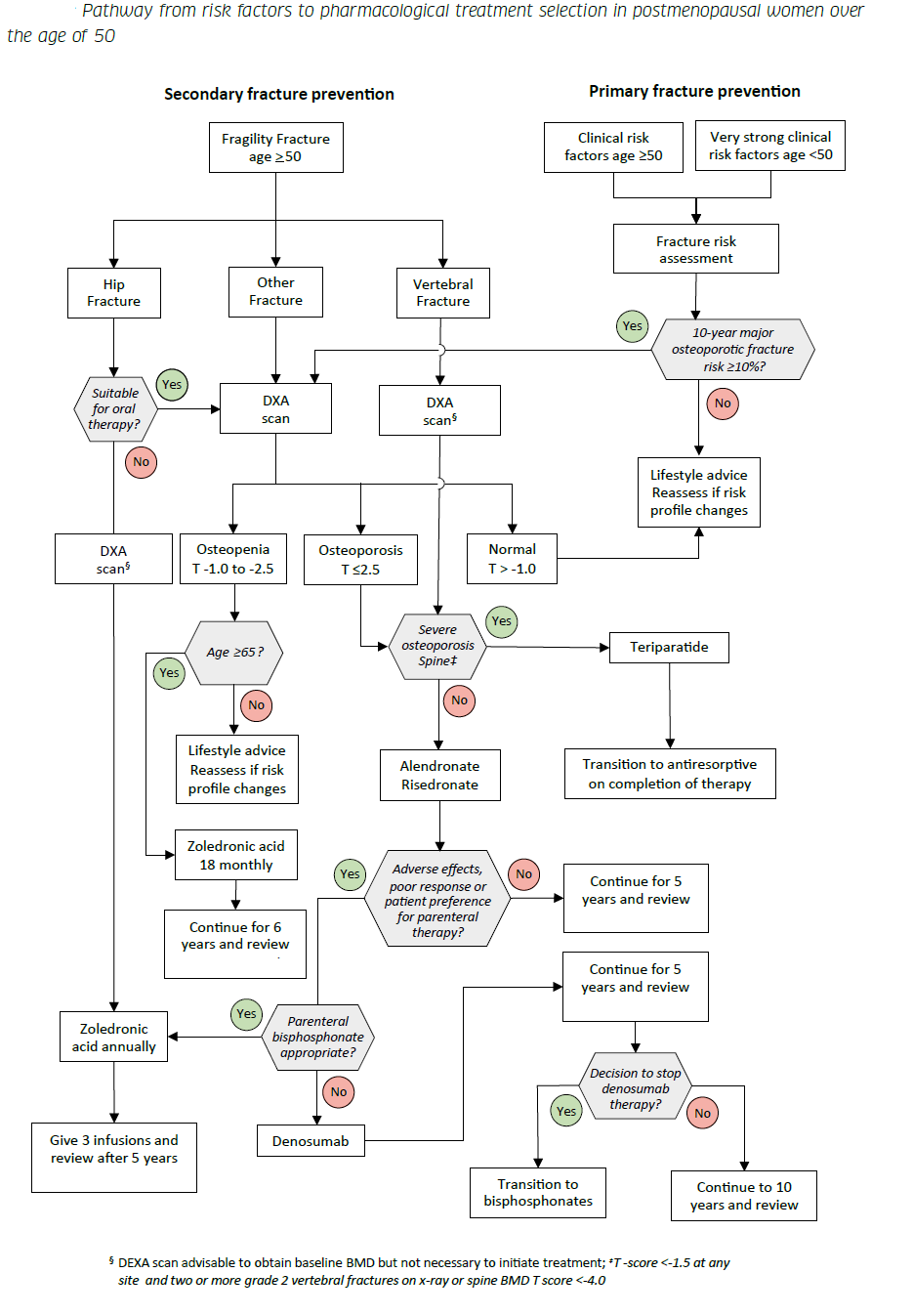
SIGN have produced an algorithm for pharmacological treatment selection in prostmenopausal women over age 50 - of note is that if a fragility fracture in a women >=65 years and osteopenia then treatment with zolendronic acid is suggested (1)
Notes:
- Zoledronic acid is recommended to prevent vertebral, non-vertebral and hip fractures in postmenopausal women with pre-existing vertebral fractures and/or DXA-proven
osteoporosis - Zoledronic acid is recommended to prevent further fractures in postmenopausal women with recent hip fractures who are unable or unwilling to take oral osteoporosis treatments,
without undertaking BMD measurements if these are felt to be inappropriate or impractical. - Zoledronic acid may be considered to reduce risk of clinical fractures in women over 65 years of age who have osteopenia at hip or femoral neck on DXA
- licensed regimen for zoledronic acid is annual 5 mg infusions, but infusions of the same dose every 18 months (off label) are also effective at reducing fracture risk.
Duration of treatment
Alendronic acid may be continued for up to 10 years in postmenopausal women with osteoporosis, especially those that are at high risk of vertebral fracture
Risedronate may be continued for up to seven years in postmenopausal women with osteoporosis
Zoledronic acid (5 mg, intravenously) annually for three years is recommended in postmenopausal women with osteoporosis. The clinical benefit of annual zoledronic acid
in preventing fractures beyond three years is uncertain.
Strontium ranelate may be continued for up to 10 years in postmenopausal women with severe osteoporosis when other treatments are unsuitable.
Denosumab should be continued for five years for treatment of patients with osteoporosis and may be continued for up to 10 years in patients at high risk of fracture.
Monitoring pharmacological effect
- repeat BMD measurements by DXA after an interval of three years may be considered to assess response to treatment in postmenopausal women on alendronic acid, ibandronic acid, zolendronic acid or denosumab therapy.
Details regarding treatment options:
- alendronic acid is recommended to prevent vertebral fractures, non-vertebral fractures and hip fractures in postmenopausal women with pre-existing vertebral fractures and/or DXA-proven osteoporosis
- risedronate is recommended to prevent vertebral fractures, non-vertebral fractures and hip fractures in postmenopausal women with pre-existing vertebral fractures and/or DXA-proven osteoporosis
- zoledronic acid
- recommended to prevent vertebral, non-vertebral and hip fractures in postmenopausal women with pre-existing vertebral fractures and/or DXA-proven
osteoporosis - recommended to prevent further fractures in postmenopausal women with recent hip fractures who are unable or unwilling to take oral osteoporosis treatments, without undertaking BMD measurements if these are felt to be inappropriate or impractical
- may be considered to reduce risk of clinical fractures in women over 65 years of age who have osteopenia at hip or femoral neck on DXA
- licensed regimen for zoledronic acid is annual 5 mg infusions, but infusions of the same dose every 18 months (off label) are also effective at reducing fracture risk
- recommended to prevent vertebral, non-vertebral and hip fractures in postmenopausal women with pre-existing vertebral fractures and/or DXA-proven
- ibandronic acid
- oral ibandronic (150 mg monthly) may be considered to prevent vertebral fractures in postmenopausal women with DXA-proven osteoporosis
- intravenous ibandronic acid (3 mg every three months) may be considered to prevent vertebral fractures in postmenopausal women with DXA-proven osteoporosis who are
intolerant of oral therapy or those in whom adherence to oral therapy may be difficult
- strontium ranelate
- may be considered for the treatment of severe postmenopausal osteoporosis to reduce the risk of vertebral and non-vertebral fractures in patients without established cardiovascular disease when other treatments are contraindicated
- may be considered for the treatment of severe postmenopausal osteoporosis to reduce the risk of vertebral and non-vertebral fractures in patients without established cardiovascular disease when other treatments are contraindicated
- denosumab
- recommended to prevent vertebral, non-vertebral and hip fractures in postmenopausal women with DXA-proven osteoporosis for whom oral bisphosphonates are unsuitable due to contraindication, intolerance or inability to comply with the special administration instructions
- serum calcium should be checked two weeks before denosumab treatment is due, for all patients. Patients with renal impairment (eGFR <30 ml/min) should have serum calcium checked again two weeks after therapy
- teriparatide (parathyroid hormone 1-34)
- recommended to prevent vertebral and non-vertebral fractures in postmenopausal women with severe osteoporosis
- in postmenopausal women with at least two moderate or one severe low-trauma vertebral fractures, teriparatide is recommended over oral bisphosphonates, to prevent vertebral fracture
- teriparatide discontinuation is associated with bone loss, treatment with an antiresorptive agent should be considered to maintain the increase in bone density once a course of teriparatide has been completed
- hormone replacement therapy
- hormone replacement therapy may be considered for the prevention of vertebral, nonvertebral and hip fractures in younger postmenopausal women
- before initiating HRT healthcare professionals should assess every woman’s overall risk, including cardiovascular risk, particularly in those aged over 60 who have increased baseline risk of serious adverse events
- for all women, the lowest effective dose of HRT should be used for the shortest time (1)
- tibolone
- may be considered to prevent vertebral and non-vertebral fractures in younger postmenopausal women, particularly those with menopausal symptoms
- may be considered to prevent vertebral and non-vertebral fractures in younger postmenopausal women, particularly those with menopausal symptoms
- raloxifene
- may be considered as a treatment option for the prevention of vertebral fractures in postmenopausal women when other treatments are contraindicated or unsuitable
Reference:
- SIGN (June 2020). Management of osteoporosis and the prevention of fragility fractures
Related pages
- Hormone replacement therapy (in osteoporosis)
- Tibolone
- Bisphosphonates in the treatment of osteoporosis
- NICE guidance - bisphosphonates , strontium ranelate , raloxifene and teriparatide for the secondary prevention of fractures in osteoporotic postmenopausal women
- Combined calcium and vitamin D supplements in osteoporosis
- Calcitonin in osteoporosis
- Strontium ranelate for osteoporosis
- Calcitriol in osteoporosis
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.