Antibiotics in acute otitis media
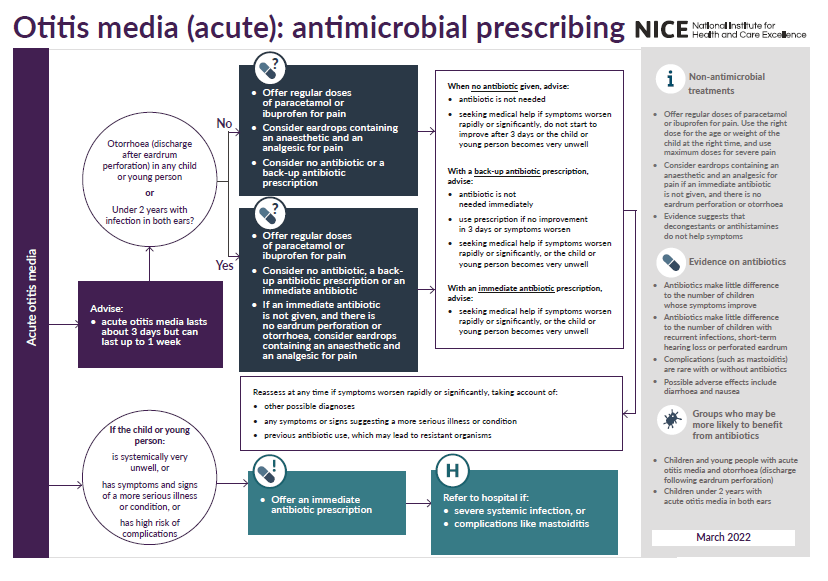
Public Health England guidance suggests (1):
- regular paracetamol or ibuprofen for pain (right dose for age or weight at the right time and maximum doses for severe pain)
- criteria for antibiotic use:
- if otorrhoea or under 2 years with infection in both ears
- then consider no antibiotic, back-up antibiotic or immediate antibiotic
- if no otorrhoea or under 2 years with infection in one ear or 2 years or older with ear infection (in one or both ears)
- then consider no antibiotic or back-up antibiotic
- if systemically very unwell or high risk of complications
- requires immediate antibiotic
- requires immediate antibiotic
- if otorrhoea or under 2 years with infection in both ears
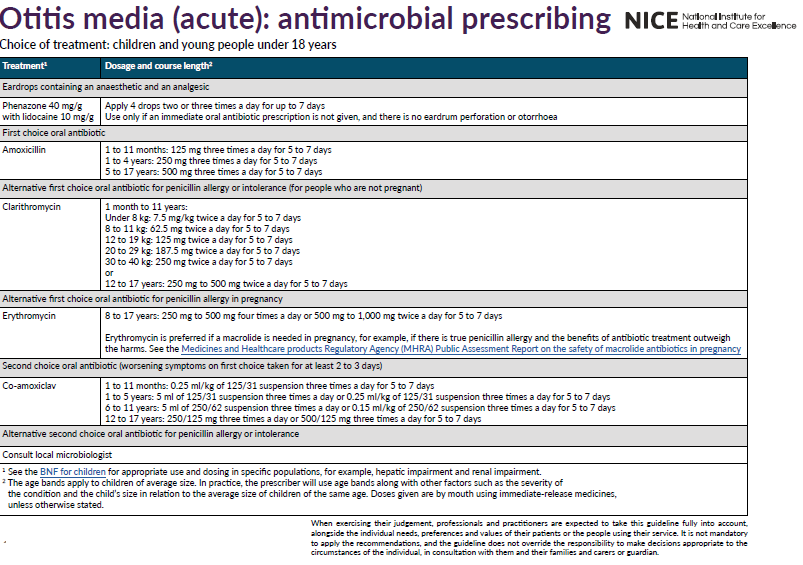
- choice of antibiotic:
- First choice: amoxicillin for 5 to 7 days
- Penicillin allergy: clarithromycin for 5 to 7 days (but erythromycin is preferred if pregnant)
- Second choice: co-amoxiclav
NICE have produced a summary of antibiotic prescribing in otitis media (2)
Erythromycin is an alternative for penicillin allergic patients, although it is less effective against Haemophilus influenzae, which is the cause of AOM in around 25% of people (3)
- azithromycin and clarithromycin are alternatives that are effective against all the main pathogens that cause AOM
Some studies suggest that antibiotics are associated with a reduction of middle ear effusions, particularly when they are unilateral, three months post treatment.
Antibiotics used in AOM do not affect:
- the recurrence rate of otitis media
- the referral rate for ENT problems
- prevalence of middle ear effusions at one month
Pain and crying drops off markedly, whether or not the child is treated with antibiotic from the beginning of the second day.
Effectiveness of antibiotic treatment in AOM
An extensive review of the use of antimicrobials in acute otitis media concluded that the evidence from randomised, placebo controlled trials that routine use of antimicrobials decreases the severity and duration of symptoms and prevents complications is weak (4)
- two thirds of children had no pain 24 hours after treatment started, irrespective of whether they received antibiotics or not, and 80% of children receiving placebo had spontaneously recovered from pain at two to seven days
- antibiotics achieved a further 7% absolute reduction in the risk of pain, or put another way, 15 children needed to be treated with antibiotics to prevent one extra child from having pain after two to seven days
Children under the age of 2 years (5)
- meta-analysis (six RCTs, n=1,643) looked at the effects of antibiotics on pain, fever, or both, at three to seven days in children aged from 6 months to 12 years with otitis media to try to find which subgroups of children were most likely to benefit from treatment
- found that, in children aged less than two years of age with bilateral AOM, 30% who were taking antibiotics had pain, fever or both at three to seven days, compared to 55% of controls (RR 0.64, 95%CI 0.52 to 0.80, NNT=4)
Delayed prescriptions (6)
- a study in an American emergency department randomised children aged six months to 12 years (n=283) who were diagnosed with AOM to an immediate or delayed prescription (after 48 hours if required) for antibiotics
- found that 62% of delayed prescriptions were not used compared with 13% of immediate prescriptions (P<0.001)
- at four to six days, an immediate prescription reduced the mean number of days of earache by just 0.4 days compared with the delayed prescription group (2.0 days vs. 2.4 days, RR 0.43, 95% CI 0.07 to 0.80)
- no statistically significant difference between the groups in the number of days of fever
In conclusion (3):
- antibiotic treatment should not be offered routinely in children with AOM
- parents can be reassured that AOM is a self-limiting illness and serious complications are rare
- antibiotics may be useful for some patients where the benefits may outweigh the risks of adverse effects (e.g. children under two years of age, those who are systemically unwell, or those who have recurrent infections)
- strategy of watchful waiting and use of delayed prescriptions may be appropriate for many children
- paracetamol or ibuprofen can be used for symptomatic relief of pain and fever.
Notes:
- a systematic review concluded that topical quinolones are better than systemic antibiotics for chronic suppurative otitis media (7)
- AOM resolves in 60% in 24hrs without antibiotics, which only reduce pain at 2 days (NNT 15) and does not prevent deafness (3)
- antibiotics to prevent Mastoiditis NNT >4000
Reference:
- Public Health England (June 2021). Managing common infections: guidance for primary care
- NICE (March 2022). Otitis media (acute): antimicrobial prescribing
- Marchisio P, Galli L, Bortone B, et al; Updated Guidelines for the Management of Acute Otitis Media in Children by the Italian Society of Pediatrics: Treatment. Pediatr Infect Dis J. 2019 Dec;38(12S Suppl):S10-S21.
- Glasziou PP, Del Mar CB, Sanders SL, et al. Antibiotics for acute otitis media in children. Cochrane Database of Systematic Reviews 2004, Issue 1. Art. No.: CD000219.
- Rovers MM, Glasziou P, Appelman CL, et al. Antibiotics for acute otitis media: a meta-analysis with individual patient data. Lancet 2006;368:1429-35.
- Spiro DM, Tay K-Y, Arnold DH, et al. Wait-and-see prescription for treatment of acute otitis media. A randomized controlled trial. JAMA 2006;296:1235-41
- Macfadyen CA et al. Systemic antibiotics versus topical treatments for chronically discharging ears with underlying eardrum perforations. Cochrane Database Syst REv 2006; (1): CD 005608
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.