Sick note changes from April 6th 2010 - how to use the updated sick note (fit note)
On 6 April 2010, the Forms Med 3 and Med 5 were replaced with a single revised Statement of Fitness for Work
General points:
- NHS General Practitioners are required to issue, free of charge, a Statement of Fitness for Work to patients for whom they provide clinical care
- other doctors are also required to issue Statements where appropriate to patients for whom they provide clinical care
- you do not need to issue a Statement to a patient until they have been off work for more than 7 calendar days
- the Statement may be issued:
- on the day that you assessed your patient;
- on a date after you assessed your patient if you consider that it would have been reasonable to issue a Statement on the day of the assessment; or
- after consideration of a written report from another doctor or registered health care professional
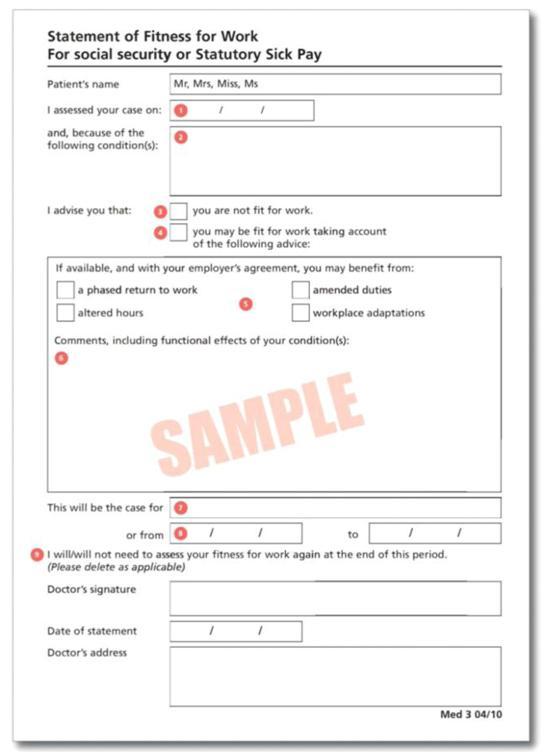
- 1) date on which you assessed your patient
- that is the date on which you either undertake or undertook:
- a face to face consultation;
- a telephone consultation; or
- the consideration of a written report from another doctor or registered healthcare professional
- Statement may be issued:
- on the day that you assessed your patient;
- on a date after you assessed your patient if you consider that it would have been reasonable to issue a Statement on the day of the assessment; or
- after consideration of a written report from another doctor or registered health care professional
- that is the date on which you either undertake or undertook:
- 2) condition or conditions that affect your patient's fitness for work
- this should be as accurate a diagnosis as possible, unless you consider that providing a precise diagnosis would be harmful to your patient's wellbeing or compromise your patient's position with their employer
- this should be as accurate a diagnosis as possible, unless you consider that providing a precise diagnosis would be harmful to your patient's wellbeing or compromise your patient's position with their employer
- 3) tick this box if your assessment of your patient is that they have or had a health condition that prevents or prevented them from working for a stated period of time
- 4) tick this box if your assessment is that your patient's condition does not necessarily stop them from returning to work
- However, they may, for example, not be able to complete all of their normal duties or could benefit from amended working hours
- However, they may, for example, not be able to complete all of their normal duties or could benefit from amended working hours
- 5) the four tick boxes represent common approaches to aid a return to work. Where the 'may be fit for work' box has been ticked, you can tick one or more of these optional tick boxes if you feel it could help your patient return to work. This list is not exhaustive and other approaches can be suggested in the comments box
- advice in comments box if fit for work
- when advising patients that they 'may be fit for work', the advice in the comments box should describe the limitation(s) that the person may have and should not be too prescriptive about the solution(s). For example, you might advise that a person with lower back pain "cannot sit for long periods of time" rather than "should be provided with a better chair" or that a person with travel-related anxiety might benefit from "avoiding travel in peak hours" rather than "should work between 10am and 4pm"
- similarly, if your patient will need a specialist referral that may need time off work to attend, it will be helpful to your patient and their employer to note this in the comments box. For example, you might advise that your patient "has been referred for physiotherapy which may require time off to attend"
- advice in comments box if fit for work
- 6) where the 'may be fit for work' box has been ticked, you must complete this section with information on the functional effects of your patient's condition. The information you provide here will be key for your patient and for their employer when they are considering if and how they can facilitate a return to work. In circumstances where you feel the issues are complex or where you feel work itself may be a contributor to your patient's condition you may wish to include in your comments a recommendation that an occupational health assessment be considered
- 7) specify here how long the advice is for. This will be from the date of assessment. During the first 6 months of sickness this can be up to a maximum of 3 months. After the first 6 months of incapacity, a Statement can be issued for any clinically appropriate period up to 'an indefinite period'
- 8) use this section to indicate the period the advice covers when you need to state a specific start and end date on the Statement. You will need to use this section when;
- the Statement covers a period based on a previous assessment for which no Statement has been issued; or
- the Statement is for less than 14 days and you do not need to see your patient again; or
- you believe it will be helpful to state a specific date for your patient to return to work as a motivating factor in their recovery
- 9) state here if you need to assess your patient's fitness for work again at the end of the Statement period. If you request to see your patient again and in the subsequent consultation you feel they are able to return to work without any functional limitations, you do not need to issue to them with a new Statement
The Department for Work and Pensions (DWP) amended legislation, with effect from 1 July 2022 to enable nurses, occupational therapists, pharmacists and physiotherapists to certify fit notes in addition to doctors (these five professions are referred to in this guidance as healthcare professionals - HCPs). The legislation is permissive, meaning that all these HCPs can legally certify a fit note, but they are not required to do so. Individuals should consider their scope of practice and ensure they have the relevant skills, knowledge and experience before undertaking health and work conversations and making decisions around certifying fit notes.
Legislation
- A statement of fitness for work, commonly known as a fit note or'med 3', is a form of medical evidence that can enable an individual to access health-related benefits or evidence eligibility for statutory sick pay (SSP). Its purpose, format and requirements are set out in regulations which cover England, Wales and Scotland. The fit note contains options to assess a person as 'not fit for work' or'may be fit for work taking account of the following advice'.
- The legislation requires the HCP to undertake an assessment to complete a fit note. An assessment is defined as a consultation between the patient and HCP or consideration of a written report by another health professional. The fit note provides advice about the functional effects of a patient's condition on their fitness for work but it does not require the HCP to have specialist knowledge of workplaces or occupational health or to suggest possible changes to a patient's workplace or job.
- Where patients are required to evidence eligibility for SSP, provided their employer is content, they can provide alternate forms of evidence[footnote 15]. One example of this is the'AHP Health and Work Report' [footnote 16] which can be completed by all Allied Health Professions, including those that are not legally able to certify fit notes.
Two legislative amendments were then made to improve the fit note and its use.
- Removal of the requirement for signatures in ink (April 2022). This amendment removed the barriers to fit notes being completed and certified digitally so that relevant systems could be updated to simplify the processes for completing fit notes. (Wet signature fit notes continue to be accepted.)
- Extension of certification of fit notes to a wider group of HCPs - nurses, occupational therapists, pharmacists and physiotherapists. This change legally enabled any statutorily registered member of these professions, to certify a legally valid fit note
An online training module hosted on elfh (Elearning for Health) has been developed to support HCPs in preparing to certify fit notes as part of their practice if it is an agreed part of their role.
Notes:
- form Med 10 used as evidence of a period as an inpatient is still in use and the rules and processes for this remain unaltered.
Reference:
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.