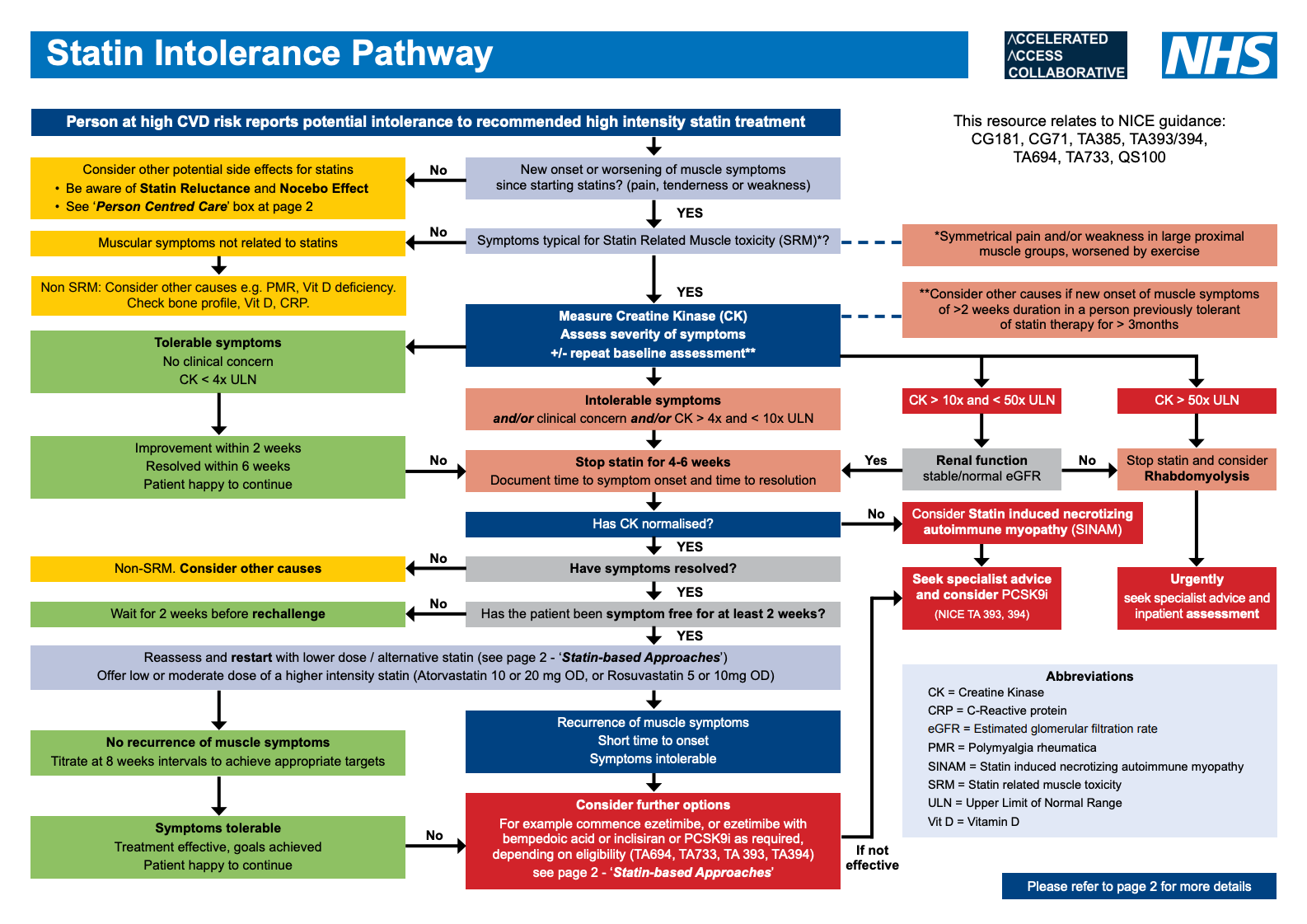
Algorithm for the management of statin intolerance
Statins are the cornerstone for prevention and treatment of cardiovascular (CV) disease with a substantial evidence of reduction of morbidity & mortality. Refer to Lipid Management Pathway and related NICE guidelines (NG238, CG71) for guidance on initiation, titration and monitoring of statin therapy.
- In clinical trials, statins were found to be largely well tolerated (often with a similar adverse effect (AE) profile to placebo), however this is not reflected in clinical practice where up to 75% of people started on a statin will discontinue treatment within 2 years
- Stopping statin therapy is associated with an increased risk of major CV events and there is growing concern that clinicians are labelling patients as ‘statin intolerant’ too quickly. Indeed statin discontinuation is significantly associated with negative media coverage
- Definition of Statin Intolerance
- Intolerance to initial statin therapy is defined by NICE as the presence of clinically significant adverse effects that represent an unacceptable risk to the patient or that may reduce compliance with therapy.
- Other definition: any adverse event (AEs) considered unacceptable by the patient, and/or some laboratory abnormalities, both attributed to statin treatment and leading to its discontinuation
- Statin-associated muscle symptoms (SAMS)
- SAMS are one of the principal reasons for statin non-adherence and/or discontinuation. However, not all such symptoms should lead to a label of ‘statin intolerance’ as they may not be truly statin related muscle toxicity (SRM) as demonstrated by resolution on de-challenge and recurrence with re-challenge
- SAMS are one of the principal reasons for statin non-adherence and/or discontinuation. However, not all such symptoms should lead to a label of ‘statin intolerance’ as they may not be truly statin related muscle toxicity (SRM) as demonstrated by resolution on de-challenge and recurrence with re-challenge
- Non-Statin related musculoskeletal symptoms (Non SRM)
- If patients report symptoms that are not typical of SRM (e.g. asymmetric distribution, failure to resolve with de-challenge despite normal CK) consider other musculoskeletal disorders, metabolic, degenerative or inflammatory e.g. Vitamin D deficiency, polymyalgia rheumatica. Check Bone profile, Vitamin D, CRP.
- If patients report symptoms that are not typical of SRM (e.g. asymmetric distribution, failure to resolve with de-challenge despite normal CK) consider other musculoskeletal disorders, metabolic, degenerative or inflammatory e.g. Vitamin D deficiency, polymyalgia rheumatica. Check Bone profile, Vitamin D, CRP.
- Considerations when starting a statin to reduce risk of SRM
- Check baseline thyroid, liver & renal function, any potential drug interactions, and avoid the highest doses in at risk groups (See “Risk Factors” below).
- Ask the person if they have had persistent generalised unexplained muscle pain, whether associated or not with previous lipid-lowering therapy. If they have, measure CK. If CK levels are > 4x ULN do not start statin - investigation required.
- Do not measure CK if person is asymptomatic.
- Warn patients about AEs, specifically muscle symptoms. Advise people who are being treated with a statin to seek medical advice if they develop muscle symptoms (pain, tenderness or weakness). If this occurs, measure CK
- Risk factors for SRM and statin intolerance
- Endogenous factors
• Female gender
• Advanced age (> 75 yrs)
• Frailty (reduced lean body mass)
• History of muscle disorder or high CK
• Impaired renal or hepatic function
• Personal or Family history of intolerance
to lipid-lowering therapies.
• Hypothyroidism - Exogenous Factors
• Excessive alcohol intake
• High intensity exercise
• Dehydration
• Drug interactions with statins
(including herbal medicines)
• Vitamin D deficiency
- Endogenous factors
- Classification of statin related muscle toxicity (SRM)
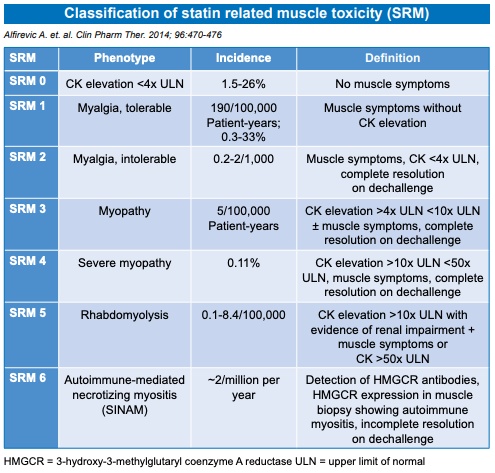
- SRM is a spectrum from myalgia to severe myopathy
- SRM 0 - does not preclude statin therapy, consider reducing starting dose
- SRM 1-3 manage according to pathway
- When SRM4 is suspected, without evidence of impaired renal function, discontinue statin therapy immediately and refer for outpatient assessment. Assess and treat possible contributory factors and re-assess the need for a statin. Intensify lifestyle modifications and consider alternative lipid lowering regimens.
- If rhabdomyolysis (SRM5) is suspected, immediately stop statins, urgently refer to inpatient assessment and management including intravenous rehydration as required to preserve renal function. Do not wait for measurement of urinary myoglobin. Post recovery, manage as for SRM4
- Statin induced necrotizing autoimmune myositis (SINAM) (SRM6) should be suspected in patients with progressive muscle weakness and ongoing CK elevation despite statin withdrawal. Requires immunosuppressive treatment and avoidance of re-exposure to statins. Re-assess the need for lipid lowering therapy - may be eligible for treatment with PCSK9 inhibitor (NICE TA 393, 394)
- Person-centred approach to address statin intolerance
- Initial Consultation
- Be aware of “nocebo effect”* and “statin reluctance”**
- Reinforce healthy lifestyle habits (e.g. exercise, reducing weight)
- Listen to the concerns of each patient.
- Explain LDL-C targets and strategies to lower LDL-C/non-HDL-C
- Discuss options to reduce LDL-C/ non-HDL-C with pros and cons
- Explain the benefits of statins
- Evaluate & identify any risk factors and address (e.g. drug interactions)
- Work with patients to identify and agree best options and next step
- (*) Nocebo effect is negative expectations of the patient regarding a treatment leading to reporting more negative effects even if they are prescribed a placebo.
- (**) Statin reluctance is an attitudinal state of aversion to taking statins (often without prior exposure)
- Follow up
- Follow up on agreed plan and address any issues / concern
- Advise patients to contact you if they experience muscle symptoms • Ongoing patient education and regular review helps addressing concerns around medicine safety and underline the importance of adherence
- Statin-based approaches to manage muscle symptoms
- Adopt person-centred approach as described above.
- Therapy with a lower dose statin is preferred to no statin
- Apply a repetitive “De-Challenge” - “Re-Challenge” approach to establish if symptoms are caused by a statin(s) and the best statin regimen for each patient
- Switch to a different statin or re-challenge with the same statin using a lower dose or frequency (intermittent dosages)
- Patients who do not tolerate statins on a daily basis, alternate day or twice-weekly dosing is a good option.
- Rosuvastatin and atorvastatin have longer half-lives, permitting their use on a non-daily regime.
- Adding ezetimibe to a lower dose statin may be better tolerated with robust reduction of LDL-C / non-HDL-C
- Once a new regime is tolerated, dose / frequency can be up-titrated slowly to achieve LDL-C / non-HDL-C goals with minimal or no muscle complaints. It is important to note that cardiovascular benefits have not been proven for all the above approaches but any reduction of LDL-C / non-HDL-C is beneficial
- Initial Consultation
LDL-C lowering options for patients with genuine statin intolerance
If genuine statin intolerance is confirmed, consider:
- Starting ezetimibe 10 mg monotherapy and assess response to treatment after 3 months. (2)
- If this does not control LDL-C adequately, use a ezetimibe 10 mg/bempedoic acid 180 mg combination. (3)
- If non HDL-C remains > 2.5mmol/L despite all other lipid lowering therapies consider using injectable therapies - such as alirocumab, evolocumab or inclisiran - by arranging a fasting blood test and assessing eligibility criteria. (4,5,6)
Reference
- Khatib R. Neely D. Statin Intolerance Pathway. On behalf of the AAC Clinical Subgroup. Jan 2022. Review date: Jan 2024. Pathway endorsed by NICE Dec 2021.
- NICE. Ezetimibe for treating primary heterozygous-familial and non-familial hypercholesterolaemia. Technology appraisal guidance TA385. Published February 2016
- NICE. Bempedoic acid with ezetimibe for treating primary hypercholesterolaemia or mixed dyslipidaemia. Technology appraisal guidance TA694. Published April 2021
- NICE. Alirocumab for treating primary hypercholesterolaemia and mixed dyslipidaemia. Technology appraisal guidance TA393. Published June 2016
- NICE. Evolocumab for treating primary hypercholesterolaemia and mixed dyslipidaemia. Technology appraisal guidance TA394. Published June 2016
- NICE. Inclisiran for treating primary hypercholesterolaemia or mixed dyslipidaemia. Technology appraisal guidance TA733. Published October 2021
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.