Melanoma is among the most common forms of cancer – and causes of cancer-related death – among young adults. Its prevalence in this group has been associated with sunbathing and sunbed use. Reducing exposure to ultraviolet light is critical in the primary prevention of melanoma. Clinical features of lesion asymmetry, border irregularity, colour variability, diameter and evolution over time should raise suspicion for melanoma and prompt further assessment with dermoscopy. In this episode, Dr Roger Henderson looks at melanoma, including the different types and how to recognise them, referral criteria, treatments and prognosis.
Key take-home points
- There are 17,500 new melanoma skin cancer cases in the UK every year, and melanoma skin cancer is the fifth most common cancer in the UK, accounting for 5% of all new cancer cases.
- Women most often develop lesions on the legs, whereas men tend to present with disease on the trunk.
- The risk of developing melanoma exists along a spectrum.
- Both cumulative lifetime sun exposure and intense, intermittent episodes such as severe sunburns are implicated, and sunbed use is particularly problematic.
- The majority of melanoma skin cancer cases in the UK are preventable.
- Around 80% of cases arise de novo on previously normal skin, while the rest develop within pre-existing moles.
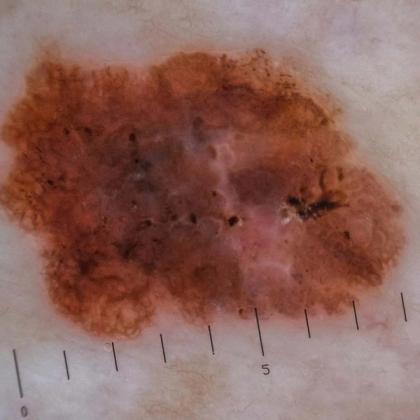
- The classic diagnostic framework still remains the ABCDE rule (asymmetry, border irregularity, colour variation, diameter >6 mm [or dimensions] and evolution).
- For nodular melanomas, the EFG rule (elevated, firm, growing) is more helpful.
- Itching and irritation are nonspecific symptoms and do not help in distinguishing benign from malignant lesions.
- Dermoscopy can significantly increase diagnostic accuracy compared with the naked eye, but this requires both training and experience.
- Superficial spreading melanomas account for around 70–80% of cases in the UK.
- Nodular melanomas are the second most common type and typically arise between the ages of 40 and 60.
- Lentigo maligna melanomas tend to occur in older patients with long-term sun damage, usually on the face or neck and often progress slowly over years.
- Acral lentiginous melanomas are rare overall but are proportionally much more common in people with darker skin and in Asian populations and occur on the palms, soles or under nails.
- Mucosal melanomas arise from melanocytes in the lips, nasal passages or genital mucosa. These account for about 2% of all melanomas, are not related to UV exposure and are aggressive with a poorer prognosis.
- NICE guidance recommends urgent referral through the suspected cancer pathway for any lesion scoring ≥3 on the weighted seven-point checklist, any pigmented or non-pigmented lesion suggestive of nodular melanoma or any lesion that appears suspicious on dermoscopy.
- Once referred, the diagnostic standard is a complete excisional biopsy with narrow margins.
- Breslow thickness (the measurement of tumour depth in millimetres) is the single most powerful predictor of survival.
- Treatment is stage-dependent.
- The introduction of immune checkpoint inhibitors, such as anti-CTLA-4 and anti-PD-1 antibodies, has transformed prognosis.
Key references
- NICE. 2022. https://www.nice.org.uk/guidance/ng14.
- PCDS. 2025. https://www.pcds.org.uk/clinical-guidance/melanoma-an-overview1.
- Balch CM, et al. J Clin Oncol. 2009;27(36):6199-6206.doi: 10.1200/JCO.2009.23.4799.
- Tas F, Erturk K. Am J Dermatopathol. 2022;44(11):799-805. doi: 10.1097/DAD.0000000000002264.
- Kozyra P, et al. Int J Mol Sci. 2022;23(11):6084. doi: 10.3390/ijms23116084.
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.