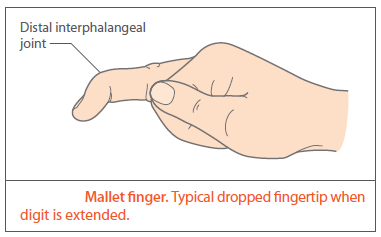
This describes the characteristic drooping of the finger observed with injury to the extensor digitorum longus at its insertion at the base of the distal phalanx.
- a mallet finger may result from direct trauma to the finger tip or more commonly, by forcibly bending the finger in extension, for example, when catching a ball - hence, the synonym, "baseball finger " (may occur in other similar sports such as netball and volleyball)
- in older patients, the associated trauma may be minor for example, catching the tip of the finger whilst changing the sheets on the bed
- the extensor mechanism is disrupted. The finger is held flexed at the distal interphalangeal joint. There is no active movement but passive movement is unimpaired. In time, the proximal phalanx may become hyperextended
- an xray should be obtained to look for any associated fracture.
Most injuries are treated conservatively. A mallet finger splint is applied to hold the distal interphalangeal extended whilst permitting movement at the proximal interphalangeal joint. The splint is typically required for 6 weeks. The injury should be reviewed after the first week as frequently, a smaller splint is required once the swelling subsides.
Mallet injuries with associated fractures should be reviewed by a hand surgeon as these may require operative treatment
- surgical treatment should be considered where the mallet finger presents as an open injury, where the bony mallet involves more than 30% of the articular surface of the joint, or if passive extension cannot be achieved (1)
Old injuries may still respond to splintage. If conservative treatment fails then operative intervention may be considered if there is marked deformity or significant impairment of hand function. Part of the tendon is excised over the terminal phalanx and the joint held extended with a Kirschner wire.
Reference:
- (1) Arthritis Research UK (April 2013). The upper limb in primary care. Part 2: Wrist, hand. Hands On 2(7).
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.