- there is no evidence to support an association between measles in pregnancy and congenital defects (1)
- however, the need for effective post-exposure protection is supported by studies suggesting a high risk of severe maternal morbidity, fetal loss and prematurity
- measles is more severe in pregnancy, and increases the risk of miscarriage, stillbirth, or preterm delivery (2)
- measles is more severe in pregnancy, and increases the risk of miscarriage, stillbirth, or preterm delivery (2)
- measles in late pregnancy can also lead to perinatal infection in the infant, which may be associated with a high mortality and the risk of subacute sclerosing panencephalitis
- UK guidance recommends using human normal immunoglobulin for susceptible pregnant women exposed to measles (1,2)
- although there is no direct evidence that this will reduce the complications of measles in pregnancy, it may attenuate disease and therefore reduce the rate of complications
- measures to identify women likely to be susceptible include assessment of age, vaccination history, and/or antibody testing
- main aim of measles PEP (post exposure prophylaxis) for pregnant women is attenuation of disease and therefore human normal immunoglobulin (HNIG) can be used (2)
- will be issued up to 6 days after exposure, allowing time for assessment of immunity status in most instances (2)
- where a second exposure occurs more than 3 weeks after a first dose of immunoglobulin, a further dose may need to be considered (2)
- however, the need for effective post-exposure protection is supported by studies suggesting a high risk of severe maternal morbidity, fetal loss and prematurity
Post exposure prophylaxis (PEP) with human normal immunoglobulin is recommended for neonates with recent in utero exposure, that is those born to mothers who develop a measles rash 6 days before to 6 days after delivery (2):
Pregnant women do not require post-exposure prophylaxis if they are inadvertently given MMR (2)
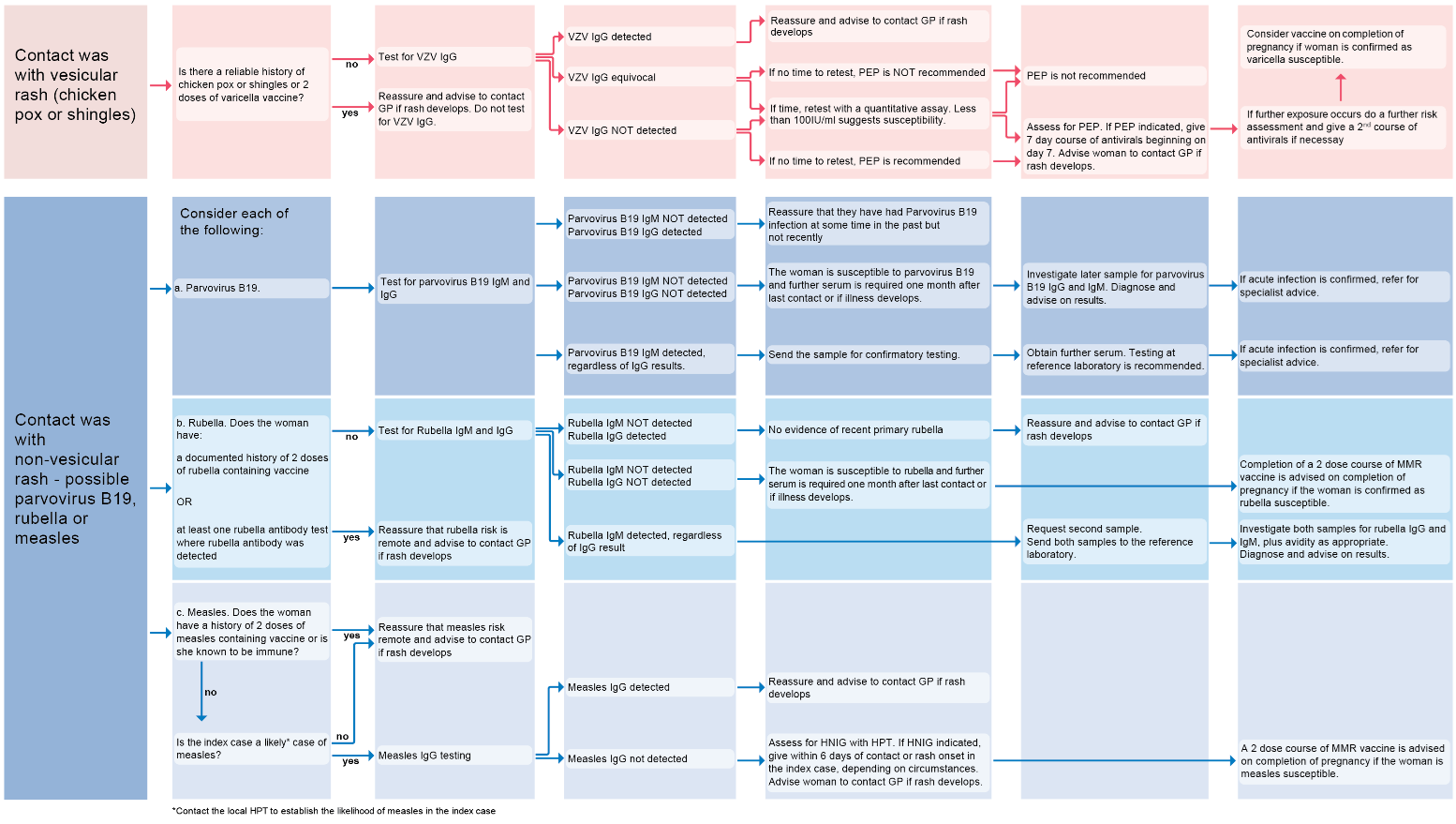
If considering an infectious cause for the development of the rash in pregnancy. A flowchart summarising contact with vesicular or non-vesicular rash (3):
Reference:
- 1) Manikkavasagan G, Ramsay M.The rationale for the use of measles post-exposure prophylaxis in pregnant women: a review. J Obstet Gynaecol. 2009 Oct;29(7):572-5.
- 2) UK Health Security Agency (July 2024). National measles guidelines
- 3) UK Health Security Agency (July 2024). Guidance on the investigation, diagnosis and management of viral illness (plus syphilis), or exposure to viral rash illness, in pregnancy
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.