Management of acute cough in primary care
Managing acute cough
The important part in the management of an acute cough is to identify whether it is an indication of a
- life threatening illness such as foreign body aspiration, pneumonia, pulmonary embolism or
- non-life-threatening diagnosis such as respiratory tract infection, exposure to allergens or irritants (1).
Consider referring the following patients to a hospital (1):
- patients with lower respiratory tract infections with severe illness
- age over 80
- cormorbidity - upper respiratory tract infection together with asthma or COPD (1)
- suspected pulmonary embolism or malignancy (1)
Be aware that an acute cough (2):
- is usually self-limiting and gets better within 3 to 4 weeks without antibiotics
- is most commonly caused by a viral upper respiratory tract infection, such as a cold or flu
- can also be caused by acute bronchitis, a lower respiratory tract infection, which is usually a viral infection but can be bacterial
- can also have other infective or non-infective causes
For children under 5 with an acute cough and fever, follow the NICE guideline on fever in under 5s: assessment and initial management.
For adults with an acute cough and suspected pneumonia, follow the NICE guideline on pneumonia in adults: diagnosis and management (3)
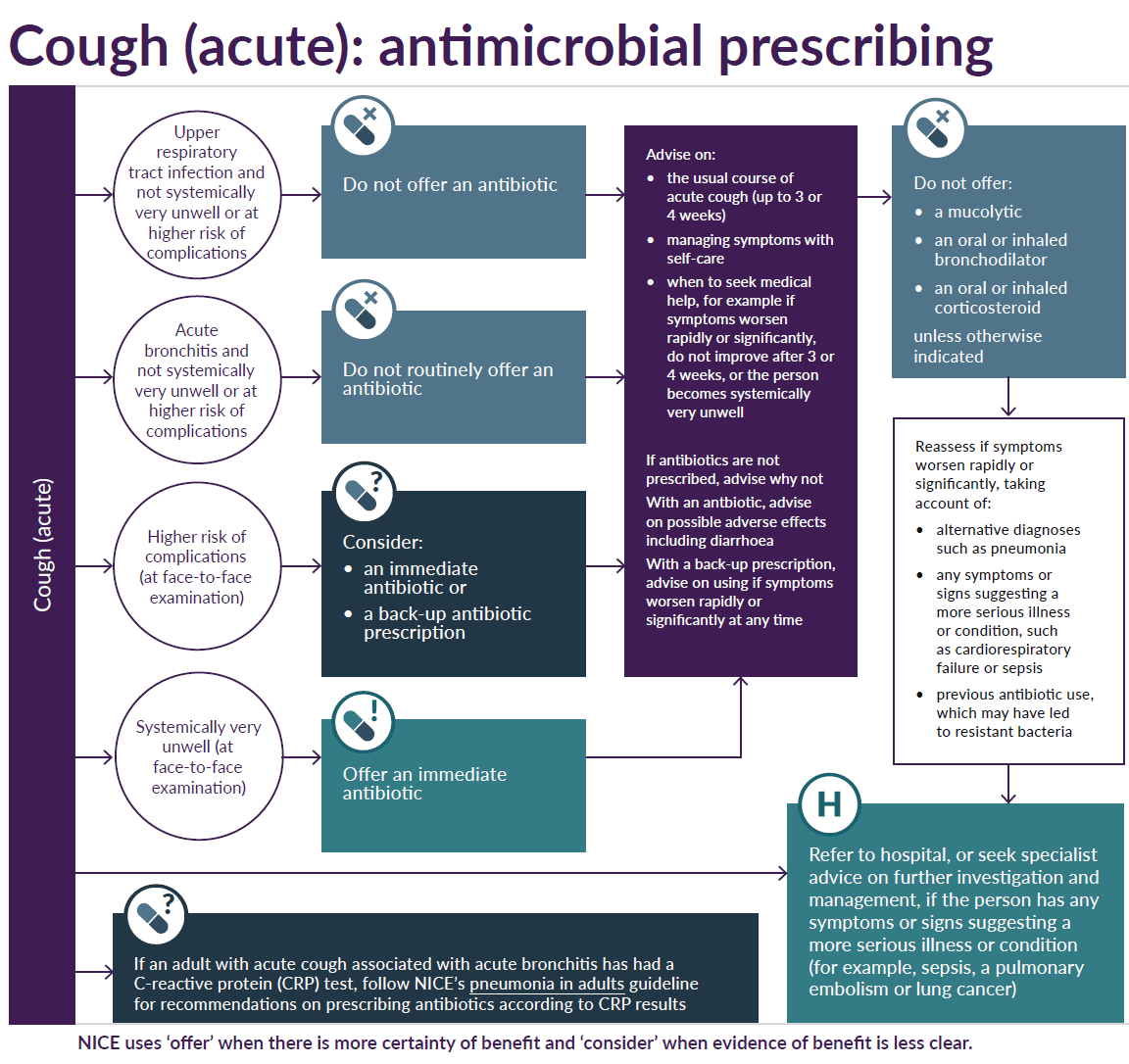
Acute cough - decision schemata (2,7):
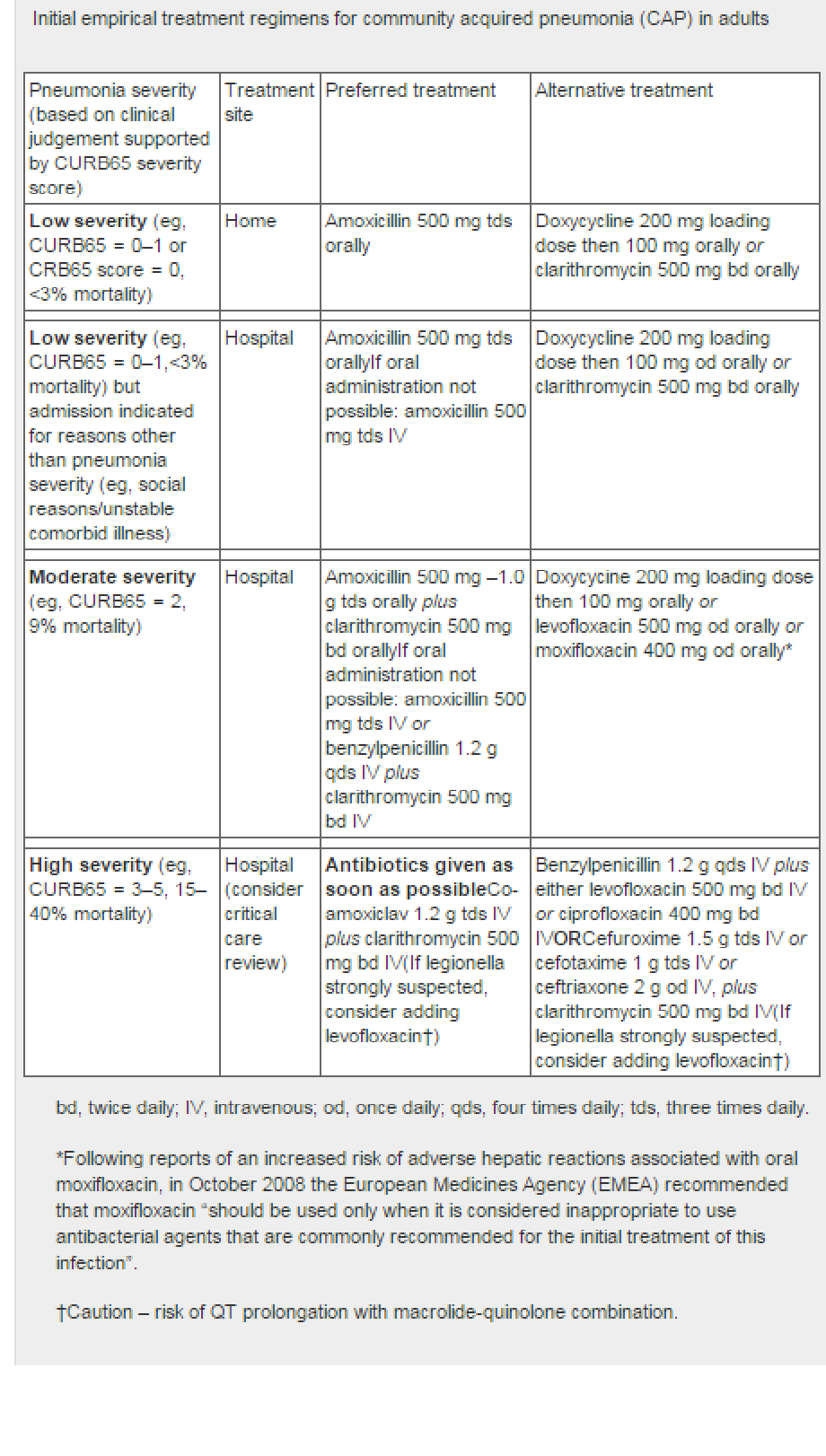
Pneumonia suspected:
- BTS guidance indicates where a patient should be treated, as well as suggested antibiotic regimen (4):
See linked item for choice of antibiotic in acute cough.
Notes:
- patients at higher risk of complications - these are defined as:
- if they:
- have a pre-existing comorbidity, such as significant heart, lung, renal, liver or neuromuscular disease, immunosuppression or cystic fibrosis
- are young children who were born prematurely
- are older than 65 years with 2 or more of the following criteria, or older than 80 years with 1 or more of the following criteria:
- hospitalisation in previous year
- type 1 or type 2 diabetes
- history of congestive heart failure
- current use of oral corticosteroids
- if they:
- the need of urgent medical admission (in an adult) can be based on the assessment of:
- respiratory rate - more than 30 breaths per minute
- blood pressure - systolic pressure <90 mmHg, or diastolic pressure <60 mmHg
- pulse - more than 130 beats per minute
- temperature
- altered level of consciousness (1,5)
- oxygen saturation level - < 92%, or central cyanosis
- peak expiratory flow rate - < 33% of predicted (6)
- reassess people with an acute cough
- if their symptoms worsen rapidly or significantly, taking account of:
- alternative diagnoses, such as pneumonia any symptoms or
- signs suggesting a more serious illness or condition, such as cardiorespiratory failure or sepsis
- previous antibiotic use, which may have led to resistant bacteria
- if their symptoms worsen rapidly or significantly, taking account of:
- referral and seeking specialist advice
- refer people with an acute cough to hospital, or seek specialist advice on further investigation and management, if they have any symptoms or signs suggesting a more serious illness or condition (for example, sepsis, a pulmonary embolism or lung cancer)
- refer people with an acute cough to hospital, or seek specialist advice on further investigation and management, if they have any symptoms or signs suggesting a more serious illness or condition (for example, sepsis, a pulmonary embolism or lung cancer)
- when an immediate antibiotic prescription is given, give advice about possible adverse effects of the antibiotic, particularly diarrhoea and nausea
- when a back-up antibiotic prescription is given, give advice about:
- an antibiotic not being needed immediately
- using the back-up prescription if symptoms worsen rapidly or significantly at any time
- Acute cough associated with an upper respiratory tract infection
- do not offer an antibiotic to treat an acute cough associated with an upper respiratory tract infection in people who are not systemically very unwell or at higher risk of complications
- do not offer an antibiotic to treat an acute cough associated with an upper respiratory tract infection in people who are not systemically very unwell or at higher risk of complications
- limited evidence suggests that antihistamines, decongestants and codeine-containing cough medicines do not help cough symptoms
Reference
- Dicpinigaitis PV et al. Acute cough: a diagnostic and therapeutic challenge. Cough. 2009;5:11
- NICE (February 2019). Cough (acute): antimicrobial prescribing
- NICE (December 2014).Pneumonia- Diagnosis and management of community- and hospital-acquired pneumonia in adults
- 2015 - Annotated BTS Guideline for the management of CAP in adults (2009)
- Subbe CP. Validation of a modified Early Warning Score in medical admissions. QJM. 2001;94(10):521-6
- Scottish Intercollegiate Guidelines Network and British Thoracic Society 2009. British guideline on the management of asthma: a national clinical guideline
- Public Health England (June 2021). Managing common infections: guidance for primary care
Related pages
- Choice of antibiotic in acute cough
- Lung cancer (NICE guidance for urgent referral for suspected cancer)
- Community acquired pneumonia (CAP)
- Cough for more than 2 weeks
- Cough associated with possible serious features e.g. wt loss
- Cough medicines
- Aromatic inhalations
- Nursing upright in respiratory congestion
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.