General Principles of management of UTI in adults (no fever or flank pain) (1)
- treat women with severe/or >=3 symptoms (dysuria, haematuria, urgency, frequency)
- women mild/<=2 symptoms AND
- a) urine NOT cloudy 97% negative predictive value, do not treat unless other risk factors for infection.
- b) if cloudy urine use dipstick to guide treatment. Nitrite plus blood or leucocytes has 92% positive predictive value; nitrite, leucocytes, blood all negative 76% NPV
- c) consider a back-up / delayed antibiotic option
- women mild/<=2 symptoms AND
- always safety net
- first line: nitrofurantoin if GFR over 45ml/min
- GFR 30-45: only use if resistance & no alternative
- in treatment failure: always perform culture
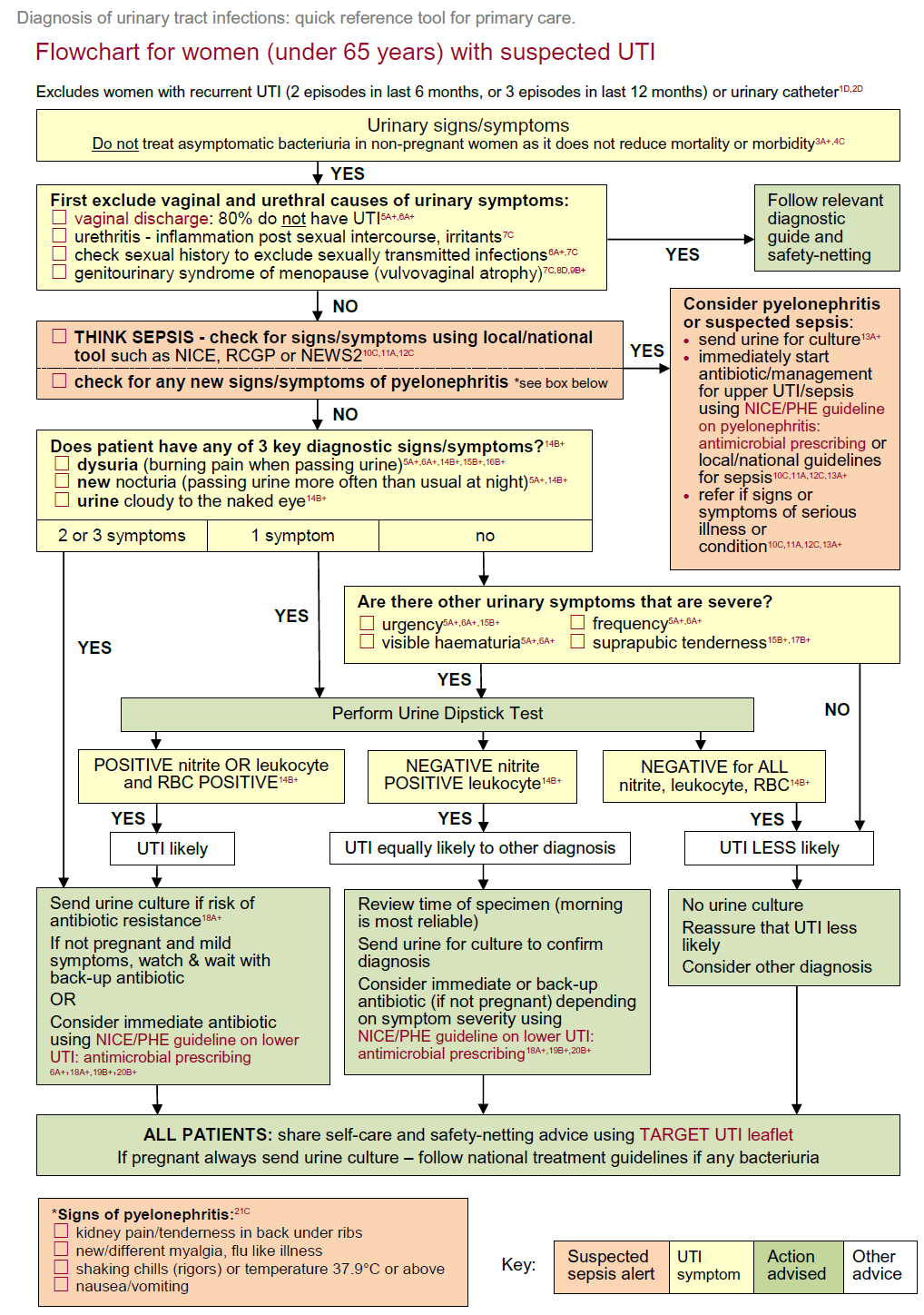
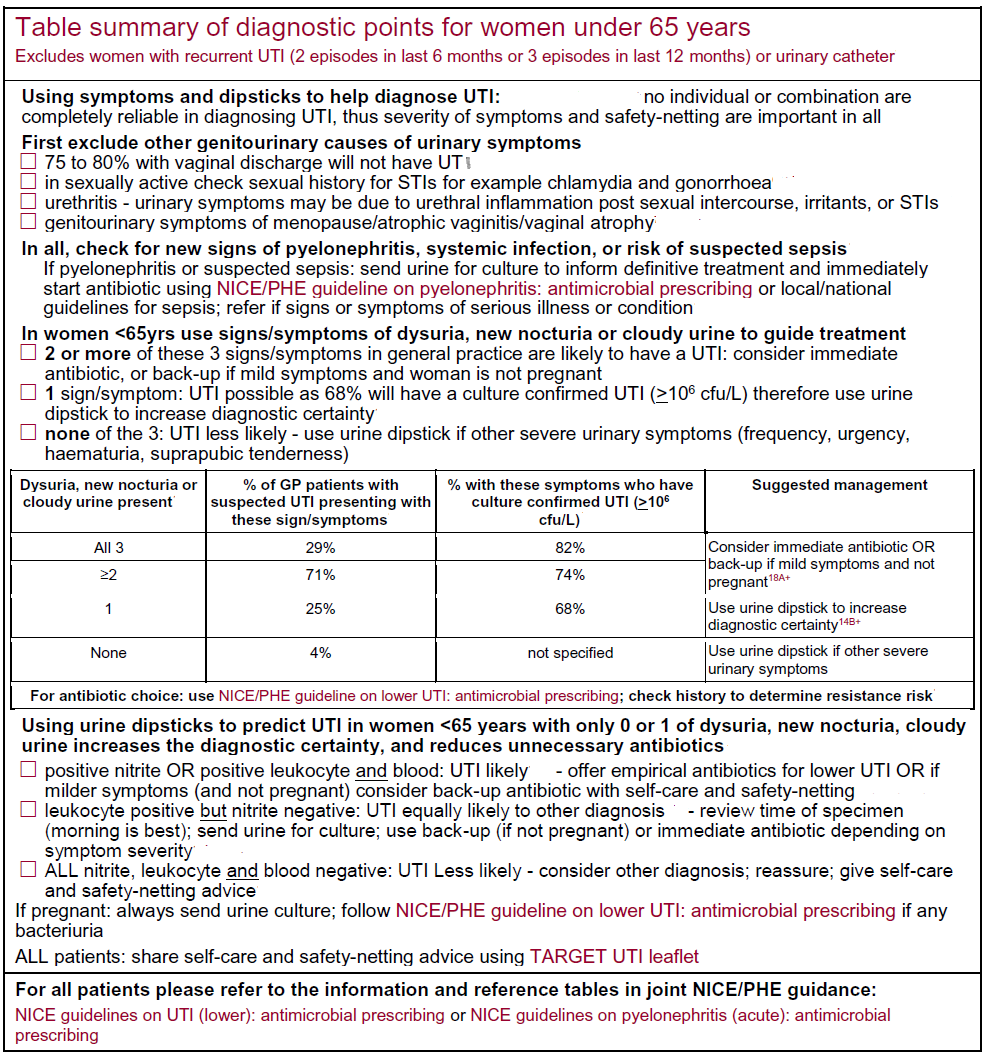
Decision tree relating to the diagnosis and management of suspected UTI in a woman under 65 years of age (2):
NICE guidance for management of UTI in an non-pregnant woman (3)
- consider a back-up antibiotic prescription or immediate antibiotic, noting that the evidence for back-up antibiotics was from women not needing immediate treatment
- if urine sent for culture and susceptibility, and antibiotic given:
- review antibiotic choice when results available, and
- change antibiotic for pregnant women if bacteria resistant
- change antibiotic for children and young people, men and non-pregnant women if bacteria resistant and symptoms not improving
- a narrow spectrum antibiotic should be used when possible
- with all antibiotic prescriptions, advise:
- possible adverse effects of antibiotics include diarrhoea and nausea
- seeking medical help if symptoms worsen at any time, do not improve within 48 hours of taking the antibiotic, or the person becomes very unwell
- with a back-up antibiotic prescription, also advise:
- antibiotic is not needed immediately
- use prescription if no improvement in 48 hours or symptoms worsen at any time
- reassess at any time if symptoms worsen rapidly or significantly or do not improve in 48 hours of taking antibiotics, sending a urine sample for culture and susceptibility if not already done. Take account of:
- other possible diagnoses
- any symptoms or signs suggesting a more serious illness or condition
- previous antibiotic use, which may have led to resistance
- Refer to hospital if a person aged 16 or over has any symptoms or signs suggesting a more serious illness or condition (for example, sepsis)
- if urine sent for culture and susceptibility, and antibiotic given:
Choice of antibiotic 1,2,3: non-pregnant women aged 16 years and over
- First choice
- nitrofurantoin - if eGFR >=45 ml/minute4
- 100 mg modified-release twice a day for 3 days
- OR
- trimethoprim - if low risk of resistance5
- 200 mg twice a day for 3 days
- nitrofurantoin - if eGFR >=45 ml/minute4
- Second choice (no improvement in lower UTI symptoms on first choice taken for at least 48 hours, or when first choice not suitable)3, 6
- nitrofurantoin - if eGFR >=45 ml/minute4 and not first choice
- 100 mg modified-release twice a day for 3 days
- OR
- pivmecillinam (a penicillin)
- 400 mg initial dose, then 200 mg three times a day for a total of 3 days
- OR
- fosfomycin
- 3 g single dose sachet
- nitrofurantoin - if eGFR >=45 ml/minute4 and not first choice
Notes:
- 1 check BNF for use and dosing in specific populations, for example, hepatic impairment, renal impairment and breast-feeding.
- 2 doses given are by mouth using immediate-release medicines, unless otherwise stated.
- 3 check any previous urine culture and susceptibility results and antibiotic prescribing and choose antibiotics accordingly.
- 4 may be used with caution if eGFR 30-44 ml/minute to treat uncomplicated lower UTI caused by suspected or proven multidrug resistant bacteria and only if potential benefit outweighs risk (BNF, August 2018).
- 5 alower risk of resistance may be more likely if not used in the past 3 months, previous urine culture suggests susceptibility (but this was not used), and in younger people in areas where local epidemiology data suggest resistance is low. A higher risk of resistance may be more likely with recent use and in older people in residential facilities.
- 6 ifthere are symptoms of pyelonephritis or the person has a complicated UTI (associated with a structural or functional abnormality, or underlying disease, which increases the risk of a more serious outcome or treatment failure), see the recommendations on choice of antibiotic in the NICE antimicrobial prescribing guideline on acute pyelonephritis.
Risk factors for increased resistance include:
- care home resident,
- recurrent UTI,
- hospitalisation >7d in the last 6 months,
- unresolving urinary symptoms,
- recent travel to a country with increased antimicrobial resistance (outside Northern Europe and Australasia) especially health related,
- previous known UTI resistant to trimethoprim, cephalosporins or quinolones
More extensive details of drug treatment are provided in the BNF (section 5.1.13).
Indwelling catheters always seem to result in white cells and bacteria which are very difficult to get rid of. Usually they are asymptomatic, and are only to be treated with the development of symptoms.
Reference:
- Public Health England (2017). Management of infection guidance for primary care for consultation and local adaptation
- Public Health England (August 2019). Diagnosis of urinary tract infections - Quick reference tool for primary care for consultation and local adaptation
- NICE (October 2018). Urinary tract infection (lower): antimicrobial prescribing
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.