Brief practical guide to HRT
Brief Practical Guide to HRT
Suggested first-line HRT regime:
Women without a uterus Transdermal oestrogen (detailed below) are have many benefits over oral oestrogen. Transdermal oestrogen preparations are available as gels or patches: Gels • Oestrogel 2-4 pumps a day, or, Patches • Evorel 25 / 50 / 75 / 100mcg patches twice a week, or, Spray Lenzetto 1-3 sprays |
Women with a uterus Transdermal oestrogen as above. Will also need progestogen - micronised progesterone (Utrogestan) has many potential benefits over other progestogens (detailed below) Utrogestan • 100mg capsule each evening as continuous (licensed for days 1-25 but easier to take every night)
|
Risks and benefits of HRT
- safety of HRT largely depends on age. Healthy women younger than 60 years should not be concerned about the safety profile of HRT (1)
- for most women, the potential benefits of HRT given for a clear indication are many and the risks are few when initiated within 10 years of menopause
- symptoms of the menopause such as hot flushes, mood swings, night sweats, and reduced libido improve (2)
Proven benefits (1):
- control of menopausal symptoms
- maintenance and improvement of BMD (bone mineral density) and reduced risk osteoporotic fractures
- reduced risk coronary heart disease
Additional Potential Benefits (1):
- Alzheimers disease when oestrogen started early
- reduced risk colorectal cancer
- reduced risk Type 2 DM (diabetes mellitus).
Known risks (1):
- endometrial cancer (if oestrogen only given when uterus present)
- reduced by addition of progestogen
- continuous progestogen provides better long-term protection than cyclical
- DVT/PE: 2-3 background risk, which is 1.7 per 1,000 women aged over 50
- greatest risk in 1st 12 months, this risk is not present with non-oral (patch, gel or spray)
- overall venous thromboembolism (VTE) risk increases about two-fold in women who take oral oestrogens
- high levels of oral oestrogen concentrate in the liver, which results in activation of the coagulation and activation factors of the renin–angiotensin–aldosterone cascade. In addition, oral (but not transdermal) oestrogens induce resistance to activated protein C
- in contrast, studies have shown no association between VTE risk and use of transdermal oestrogens (3)
- guidelines recommend transdermal rather than oral HRT for menopausal women who are at increased risk of VTE, including those with a BMI >30 kg/m2 (3)
- CHD: possibly increased when combined oral HRT started in older women(>60), or with pre-existing CHD. 1st 10 years after menopause = Cardiovascular ‘window of opportunity’
- stroke: increased when oral HRT started in older women (> 60 years)
- oral HRT containing oestrogen at either high or low doses is associated with an increased risk of ischaemic stroke, compared with non-users
- transdermal preparations containing low doses of oestrogen have not been shown to be associated with this risk (3)
- breast cancer: probably increased slightly after a minimum of 5 years' use of combined HRT, over the age of 50 - additional 3-4 cases per 1,000 women. Risk associated with oestrogen alone is very much less. Mortality is not increased
- risk of breast cancer is lower with micronised progesterone compared with synthetic progestogens
NB postmenopausal obesity or 2 or more units alcohol per day associated with greater breast cancer risk than 5 years combined HRT
Type of Progestogen - use of micronised progesterone
- progestogens used in HRT have distinctive biological and clinical profiles
- can be either a synthetic progesterone, which differs in structure from naturally occurring progesterone, or natural micronised progesterone (MP)
- MP can be prescribed either continuously or cyclically. The only current preparation available in the UK is Utrogestan® (Besins Healthcare (UK) Ltd)
Risk of venous thromboembolism
- risk of VTE is greater in women using medroxyprogesterone acetate compared with other progestogens
- risk of VTE increases by about 50% in women using oestrogen plus synthetic progestogens, compared with oral oestrogen alone
- does not appear to be this increased risk in women taking natural MP (3)
Cardiovascular risk
- there is no cardiovascular risk with MP
- MP can lower blood pressure
Risk of breast cancer
- evidence has shown that taking oestrogens combined with natural MP is not associated with an increased risk of breast cancer for the first 5 years (3)
- for women taking HRT for >5 years, risk of breast cancer was lower when taking MP compared with taking a synthetic progestogen
Endometrial Protection:
- oral natural progesterone, taken cyclically and continuously, provides endometrial protection comparable with that given by other progestogens.
How to prescribe HRT
The BMS suggests an algorithm for HRT choice as (1):
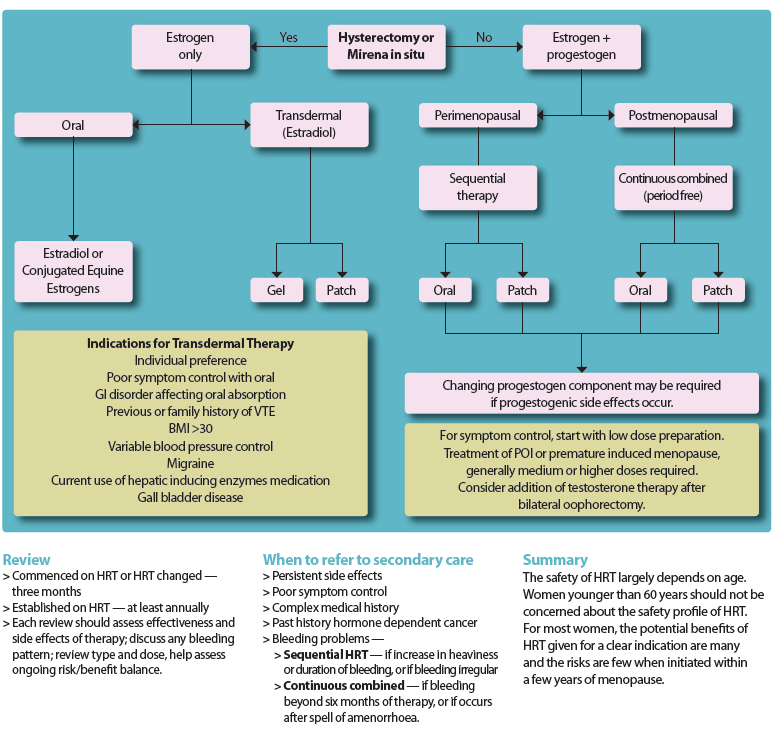
However it has also been suggested that there is robust evidence demonstrating that transdermal oestrogen in association with micronised progesterone could represent the optimal HRT regimen, particularly in women at risk of cardiovascular events (2)
Suggested that should not used combination products because:
- there is less flexibility if you want to alter the oestrogen dose
- all contain older progestogens - do not contain MP
Why transdermal oestrogen rather than oral oestrogen?
- there is increased VTE risk with oral oestrogen
- oral oestrogen increases sex hormone binding globulin (SHBG) so reduces free androgen index (lowers libido even more)
- less reliable absorption
- more contraindications (for example obesity, diabetes, gallbladder disease, migraine) with use of oral oestrogen
The most important hormone in HRT is oestrogen - best as 17 beta oestradiol (2)
The optimal dose for each woman should be given to improve symptoms and also to optimise bone and heart health. Women can continue taking HRT for as long as the benefits outweigh any risks. For most women this means they can continue taking HRT forever (4). They should have an annual review.
It is NOT about lower dose and shortest length of time anymore (2)
Detailed notes:
- Patches
- Evorel 25 / 50 / 75 / 100mcg patches twice a week
- Estradot 25 / 50 / 75 / 100mcg patches twice a week (smaller in size)
- Elleste 40 / 80mcg patches twice a week
- Gels
- Oestrogel 2-4 pumps a day (NB young women often need more)
- Sandrena gel 0.5mg sachets
- Sandrena gel 1mg sachets.
- Lenzetto 103 sprays a day
- Women with a uterus need a progestogen too
- give cyclical HRT for first year or so if they are having periods
- continuous progestogens are better for endometrial protection
- any age woman can take continuous HRT (2)
- recent evidence supports that micronised progesterone is the progestogen of choice (2,3)
- Utrogestan
- 100mg capsule each evening as continuous (licensed for days 1-25 but easier to take every night)
- 2 x 100mg capsules each evening for 2 out of 4 weeks (licensed for days 15-26 but easier to take for 2 weeks)
- can be given vaginally on alternate nights as continuous and one every night for 12-14 days each month as cyclical off license
- It is not a contraceptive. However, is women are amenorrheic taking continuous Utrogestan then it can be considered to be a contraceptive.
- Mirena - (intra-uterine system)
- Pros:
- contraception
- less risk of bleeding
- can be safely used for 5 years as endometrial protection (licensed for 4 years)
- Cons:
- systemic side effects in some women (especially
first 3-6/12) - spotting can occur in first 3-6/12
- not every woman’s choice
- not always available in primary care
- systemic side effects in some women (especially
- Pros:
- Vaginal Oestrogen
- when vaginal and/or bladder symptoms of urogenital atrophy predominate, vaginal oestrogen alone can be used.
- vaginal oestrogen may also be required in addition for some women taking systemic HRT
- tablets and creams should be used nightly for 2 weeks (3 weeks for pessary) and then twice weekly
- twice weekly maintenance doses can be continued long-term; symptoms frequently recur on cessation of therapy. Systemic absorption is minimal, and progestogen is not required.
Contributor/Reviewer:
- Dr Louise Newson,GP and Menopause Specialist (July 14th 2020)
- for further information about HRT and the menopause then see the links below:
The respective Summary of Product Characteristics (SPCs) must be consulted before prescribing any drug mentioned.
Reference:
- British Menopause Society. HRT - Guide (February 20th 2020)
- Newson LR. Easy HRT prescribing guide. Primary Care Woman's Health Forum (Accessed February 19th 2020)
- Newson LR, Lass A. Effectiveness of transdermal oestradiol and natural micronised progesterone for menopausal symptoms. BJGP 2018; 68 (675): 499-500.
- Newson LR. Review of GPnotebook "brief practical guide to HRT" (14/7/2020).
Related pages
- Hormone replacement therapy
- Topical HRT in the management of urogenital symptoms
- Alternative options for women taking sequential HRT preparations with transdermal oestradiol
- Alternative options for women taking continuous combined HRT preparations with transdermal oestradiol
- HRT - equivalence options for different doses of transdermal oestradiol
- Alternative options for women taking transdermal oestradiol only HRT in the form of (25/50/75/100) patches and do not require taking progestogen
- Alternative options for women taking a combined sequential oral HRT preparation containing 1mg of oestradiol
- Alternative options for women taking a combined sequential oral HRT preparation containing 2mg of oestradiol
- Alternative options for women taking continuous combined oral HRT preparation containing 1mg of oestradiol
- Alternative options for women taking continuous combined oral HRT preparation containing 2mg of oestradiol
- Alternative options for women taking oestrogen only (1 mg) oral HRT and do not require taking progestogen (women who had a hysterectomy)
- Alternative options for women taking oestrogen only (2 mg) oral HRT and do not require taking progestogen (women who had a hysterectomy)
- Alternatives to micronised progesterone (Utrogestan) for use in HRT
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.