Osteoporosis
Osteoporosis is a progressive, systemic skeletal disorder charcaterised by loss of bone tissue and disruption of bone micro architecture which leads to bone fragility and a consequent increased risk of fracture (1).
- bone formation exceeds bone resorption in youth, but by the third decade of life there is a gradual loss of bone mass. Hence osteoporosis is usually an age-related disease.
- in contrast to osteomalacia, the bone mineralization process is normal
It is the most common bone disease affecting the human (2)
- prevalence increases with age, it can affect both sexes, but women (especially post-menopausal women) are at greater risk because the decrease in oestrogen production after the menopause accelerates bone loss to a variable degree
- it is estimated that annually there are 180,000 osteoporosis-related symptomatic fractures in England and Wales. Of these, 70,000 are hip fractures, 25,000 are clinical vertebral fractures, and 41,000 are wrist fractures
The World Health Organization (WHO) has established diagnostic criteria for osteoporosis based on the measurement of bone mineral density (BMD), expressed as the T-score, which is the number of SD below the mean BMD of young adults at their peak bone mass:
- normal BMD: T-score of -1 SD or above
- osteopenia: T-score of between -1 and -2.5 SD
- osteoporosis: T-score of -2.5 SD or below
- established (severe) osteoporosis: T-score of -2.5 SD or below with one or more associated fractures
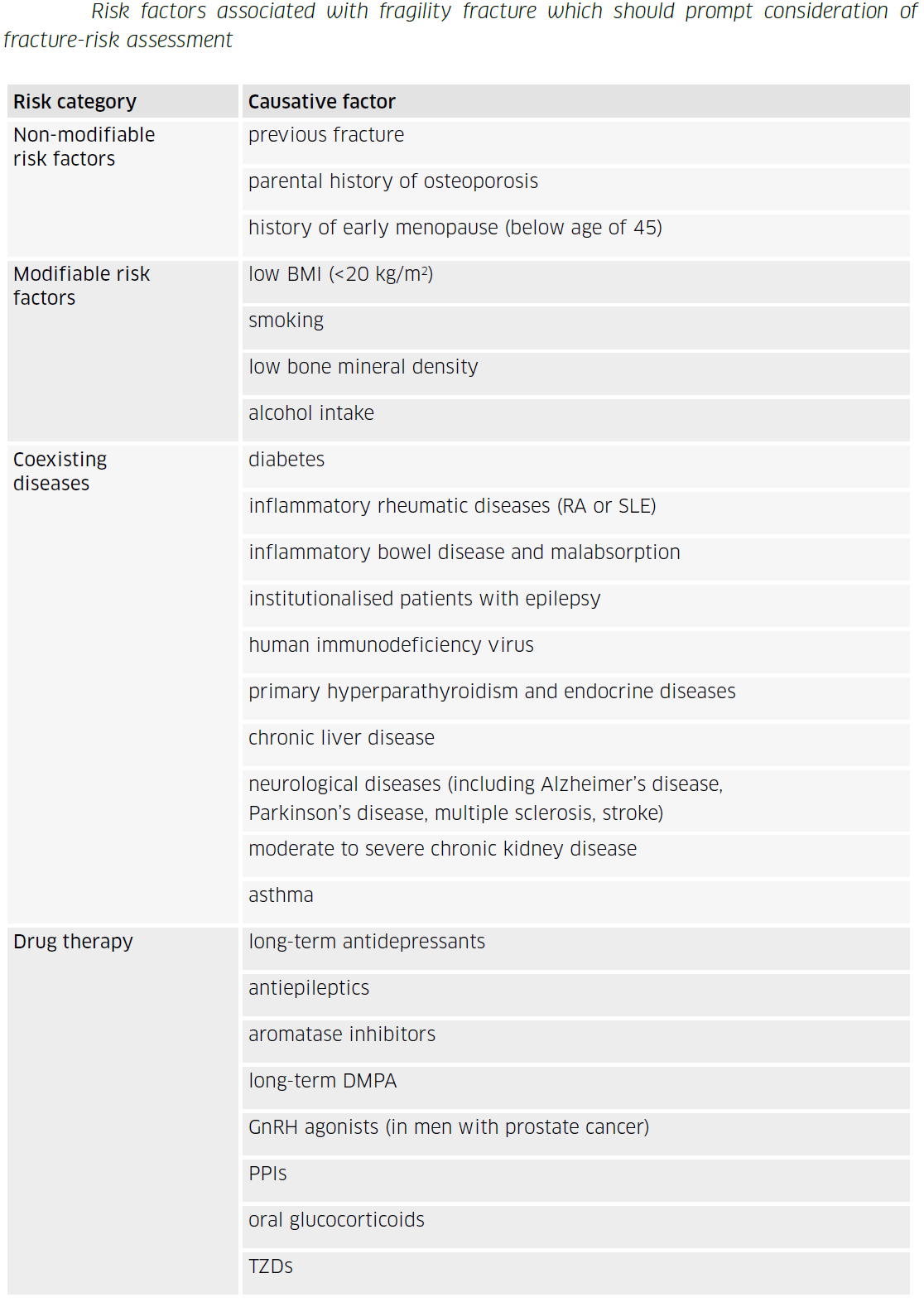
In addition to increasing age and low BMD, other clinical factors have been associated with increased fracture risk. Some of these clinical risk factors are at least partly independent of BMD, and include
- parental history of hip fracture
- alcohol intake of 4 or more units per day
- prior fracture
- long-term systemic use of corticosteroids
- rheumatoid arthritis
Factors that are known to be indicators of low BMD include low body mass index (defined as less than 22 kg/m2), and medical conditions such as ankylosing spondylitis, Crohn's disease, conditions that result in prolonged immobility, and untreated premature menopause
The American College of Physicians (ACP) recommendations on pharmacologic treatment of primary osteoporosis or low bone mass to prevent fractures in adults (4):
- recommends that clinicians use bisphosphonates for initial pharmacologic treatment to reduce the risk of fractures in postmenopausal females diagnosed with primary osteoporosis (strong recommendation; high-certainty evidence)
- suggests that clinicians use bisphosphonates for initial pharmacologic treatment to reduce the risk of fractures in males diagnosed with primary osteoporosis (conditional recommendation; low-certainty evidence)
- suggests that clinicians use the RANK (receptor activator of nuclear factor-kappaB ligand) ligand inhibitor (denosumab) as a second-line pharmacologic treatment to reduce the risk of fractures in postmenopausal females diagnosed with primary osteoporosis who have contraindications to or experience adverse effects of bisphosphonates (conditional recommendation; moderate-certainty evidence)
- suggests that clinicians use the RANK ligand inhibitor (denosumab) as a second-line pharmacologic treatment to reduce the risk of fractures in males diagnosed with primary osteoporosis who have contraindications to or experience adverse effects of bisphosphonates (conditional recommendation; low-certainty evidence)
- suggests that clinicians use the sclerostin inhibitor (romosozumab, moderate-certainty evidence) or recombinant PTH (teriparatide, low-certainty evidence), followed by a bisphosphonate, to reduce the risk of fractures only in females with primary osteoporosis with very high risk of fracture (conditional recommendation)
- suggests that clinicians take an individualized approach regarding whether to start pharmacologic treatment with a bisphosphonate in females over the age of 65 with low bone mass (osteopenia) to reduce the risk of fractures (conditional recommendation; low-certainty evidence)).
Reference:
- (1) NICE (October 2008). Alendronate, etidronate, risedronate, raloxifene and strontium ranelate for the primary prevention of osteoporotic fragility fractures in postmenopausal women
- (2) Mauck KF, Clarke BL. Diagnosis, screening, prevention, and treatment of osteoporosis. Mayo Clin Proc. 2006;81(5):662-72
- (3) SIGN (June 2020). Management of osteoporosis and the prevention of fragility fractures
- (4) Qaseem A et al. Pharmacologic Treatment of Primary Osteoporosis or Low Bone Mass to Prevent Fractures in Adults. Ann Intern Med. 2023 Jan 3. .
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.