Deep vein thrombosis, a subset of venous thromboembolism (VTE), occurs in normal veins, usually the deep calf veins of the leg and propagates more proximally (1)
- it may also affect other sites such as the upper limbs, intracranial and splanchnic veins
- anatomically, it can be divided as
- proximal DVT
- involves popliteal vein and proximal veins
- around 80% of DVTs
- distal DVT
- involves calf vein and distal veins
- the disease is often asymptomatic, but the annual incidence of symptomatic VTE is 1-2 per 1,000, of which around two-thirds are a DVT (1)
It is generally thought of as a complication of surgery or illness. (1, 2)
- surveillance data have revealed that the absolute risk of DVT in general medical patients is 10%-20% while it increases to 40%-80% in patients having hip surgery, knee surgery, or major trauma
However, a number of situations predispose an individual to a deep vein thrombosis, and are encapsulated in Virchow's Triad (blood hypercoagulability, endothelial damage and venous stasis)
The natural history is one of gradual breakdown of the thrombus with recanalisation. Damage to the valves may produce deep venous incompetence.
DVT is a usual precursor of both fatal PE and post-thrombotic syndrome (PTS) (2, 3)
References:
1. Deep vein thrombosis. NICE CKS, June 2023.
2. Venous thromboembolic diseases: diagnosis, management and thrombophilia testing. NICE Guidance (March 2020 - last updated August 2023)
3. Visona A et al. Post-thrombotic syndrome. Vasa. 2021 Sep;50 (5):331-340.
Related pages
- Epidemiology
- Predisposing factors
- Risk factors and associated increased risk for development of venous thromboembolism in surgical patients
- Clinical features
- Investigations
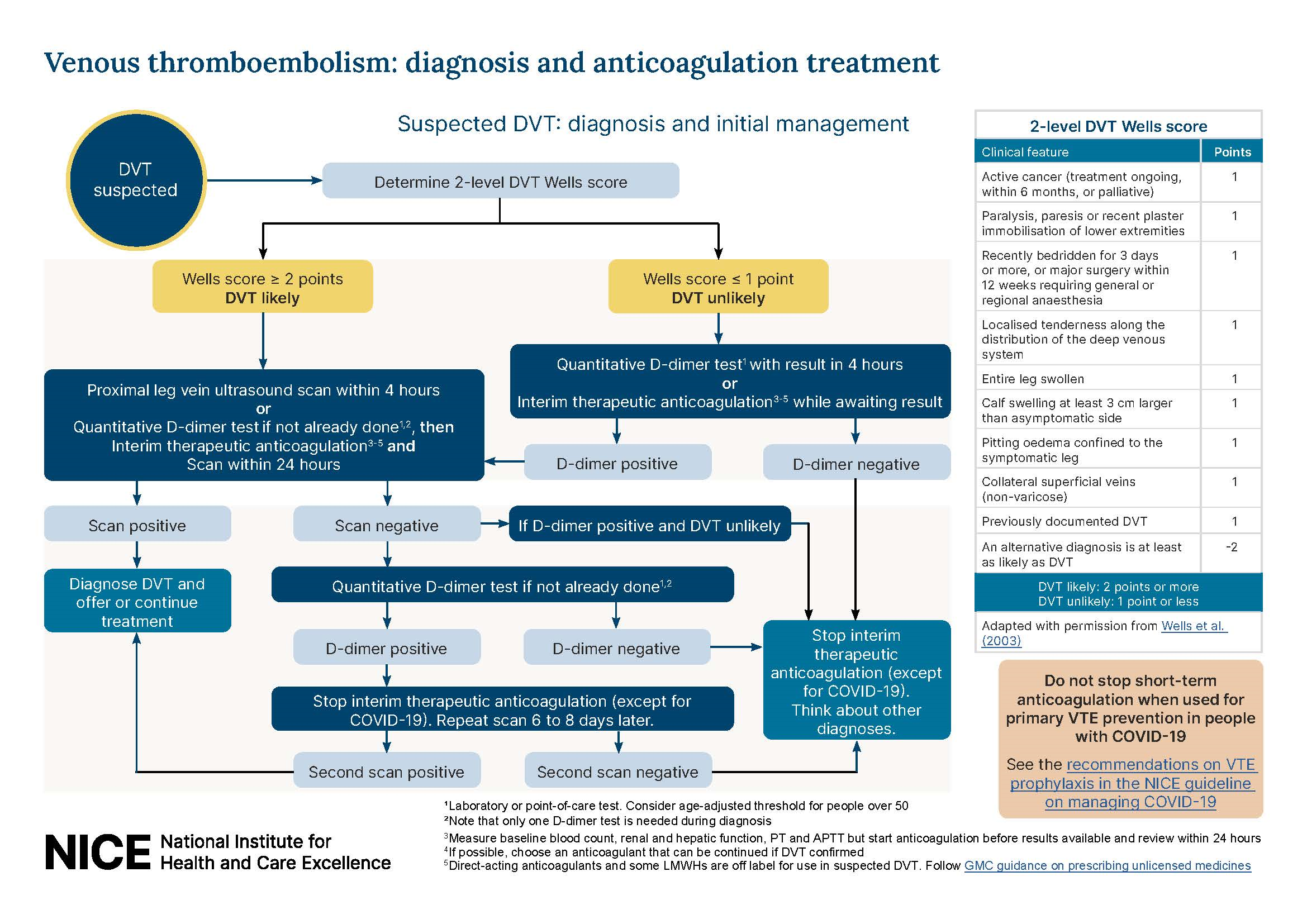
- Diagnosis of DVT
- Differential diagnosis
- Management
- Complications
- Prophylaxis versus DVT
- Risk of recurrence of thromboembolism
- Thrombophilia screen or screening
- Cancer and venous thromboembolism (VTE)
- Clinical probability of DVT
- Reducing the risk of venous thromboembolism (VTE) and air travel
- Deep vein thrombosis (DVT) in the upper extremity
- Pulmonary embolism
- Venous thromboembolism
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.