- treatment of documented lactose intolerance is removal of lactose from the diet in the form of lactose-free formulas
Low lactose diet - exclude cow’s milk and foods containing cow’s milk, although some with low lactose may be tolerated by some individuals If secondary, should resolve by 6 weeks
- children with suspected lactose intolerance do not usually require any testing and should improve within 48 hours on a low lactose diet
- in secondary lactose intolerance, for example after severe gastroenteritis, lactose can usually be tolerated again by 6 weeks (3)
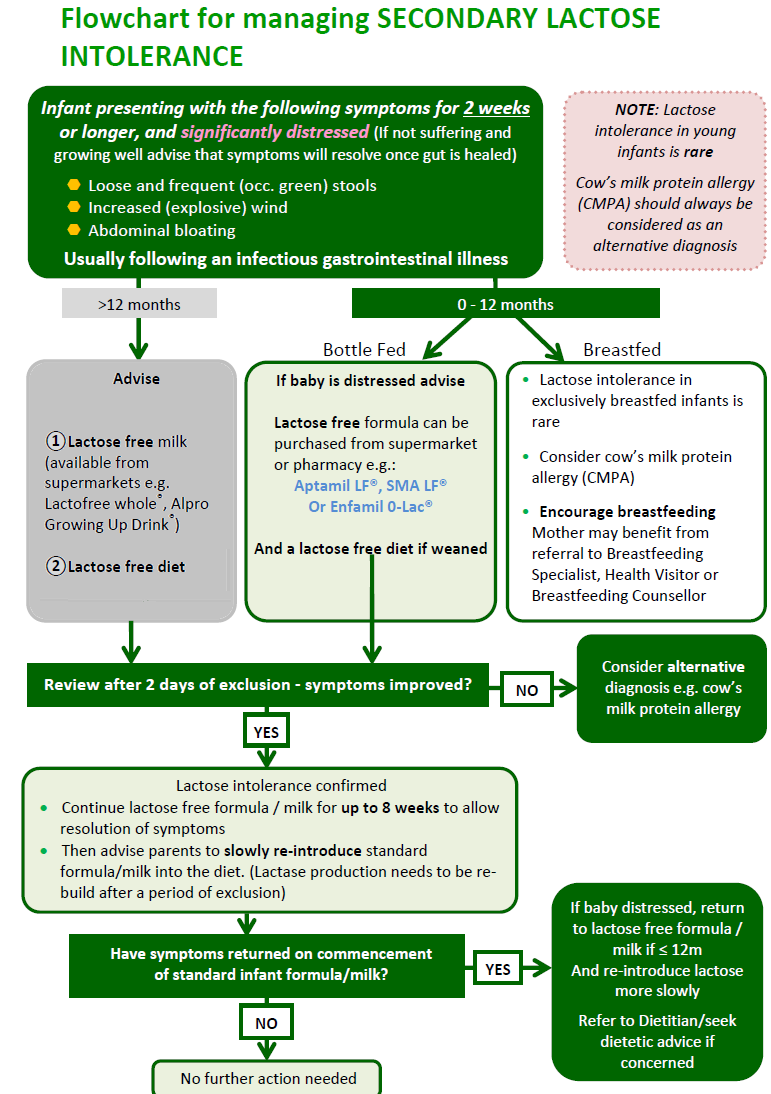
A flowchart for the management of secondary lactose intolerance has been suggested (5):
Notes:
- breastmilk contains lactose (as does any mammalian milk) and decreasing dairy intake in maternal diet does not alter the amount of lactose in breastmilk
- a baby with symptoms of lactose intolerance should not necessarily be taken off the breast and fed on special lactose-free infant formula (especially if the child is under 6 months old)
- secondary lactose intolerance is temporary, as long as the gut damage can heal. When the cause of the damage to the gut is removed, the gut will heal, even if the baby is still fed breastmilk, or their usual formula
- continuing to breastfeed (or their usual formula) will not cause any harm as long as the baby is otherwise well and growing normally (5)
- lactose-free formulae have a greater potential to cause dental caries because the non-cariogenic sugar lactose is replaced with cariogenic glucose. Therefore parents must follow good dental hygiene
Reference:
- 1. Host A., Clinical course of cow's milk protein allergy and intolerance. Pediatr Allergy Immunol 1998; 9 (Suppl 11):48-52
- 2. Wilson J. Milk Intolerance: Lactose Intolerance and Cow's Milk Protein Allergy. Newborn and Infant Nursing Reviews 2005; 5 (4): 203-207.
- 3. Walsh J et al. Differentiating milk allergy (IgE and non-IgE mediated) from lactose intolerance: understanding the underlying mechanisms and presentations. Br J Gen Pract 2016; DOI: 10.3399/bjgp16X686521
- 4. Ludman S, Shah N, Fox AT. Managing cow’s milk allergy in children. BMJ 2013; 347: f5424.
- 5.Wessex Infant Feeding Guidelines and Appropriate Prescribing of Specialist Infant Formulae (Accessed 8/3/2020)
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.