Type 2 diabetes and intercurrent illness
Last reviewed dd mmm yyyy. Last edited dd mmm yyyy
TYPE 2 DM
This guideline is not intended to serve as a protocol or standard of care:
- this is best practice based on all clinical data available for an individual case and may be subject to change as scientific knowledge and technology advances and patterns of care evolve. Adherence to guideline recommendations will not ensure a successful outcome in every case, nor should it be construed as including all proper methods of care or excluding other acceptable methods of care aimed at the same result. Ultimately a judgement must be made by the appropriate healthcare professional(s) responsible for a particular clinical procedure or treatment plan following discussion with the patient, covering the diagnostic and treatment options available. It is advised that any significant departure from the guideline should be documented in the patient’s medical record at the time the decision is taken.
Examples of intercurrent illness where "sick day rules" would be considered (1):
The following list of such illnesses is not exhaustive:
- the common cold
- influenza
- coronavirus (COVID)
- diarrhoea and vomiting
- urinary tract infection
- chest infection
- pneumonia
- abscess
- injury (e.g. fracture)
General advice for managing diabetes during intercurrent illness (1)
S (Sugar)
- Blood glucose levels can rise during illness even if the person is not eating
- Advise to increase blood glucose monitoring if the person has access to it
- Diabetes medications (sulfonylureas and insulin doses) may need to be increased temporarily during illness to manage these raised glucose levels
I (Insulin)
- NEVER stop insulin
- Insulin doses may need to be increased during illness, especially if ketones are present
- Specific advice for people on insulin therapy is presented below
- Specific advice for people on oral diabetes medication is presented below
C (Carbohydrate)
- Ensure the person maintains hydration and carbohydrate intake
- If the person is not able to eat or is vomiting, advise to replace meals with sugary fluids
- If blood glucose levels are high, maintain fluid intake with sugar-free fluids
- If blood glucose levels are low, encourage regular intake of sugary fluids
K (Ketones)
- In type 1 diabetes, advise to check for ketones every 2–4 hours
- Give extra rapid-acting insulin doses (in addition to regular doses) based on total daily
- insulin dose if ketones are present – see insulin algorithm below
- Advise to drink plenty of water to maintain hydration and flush through ketones
With respect to diabetic medications (5):
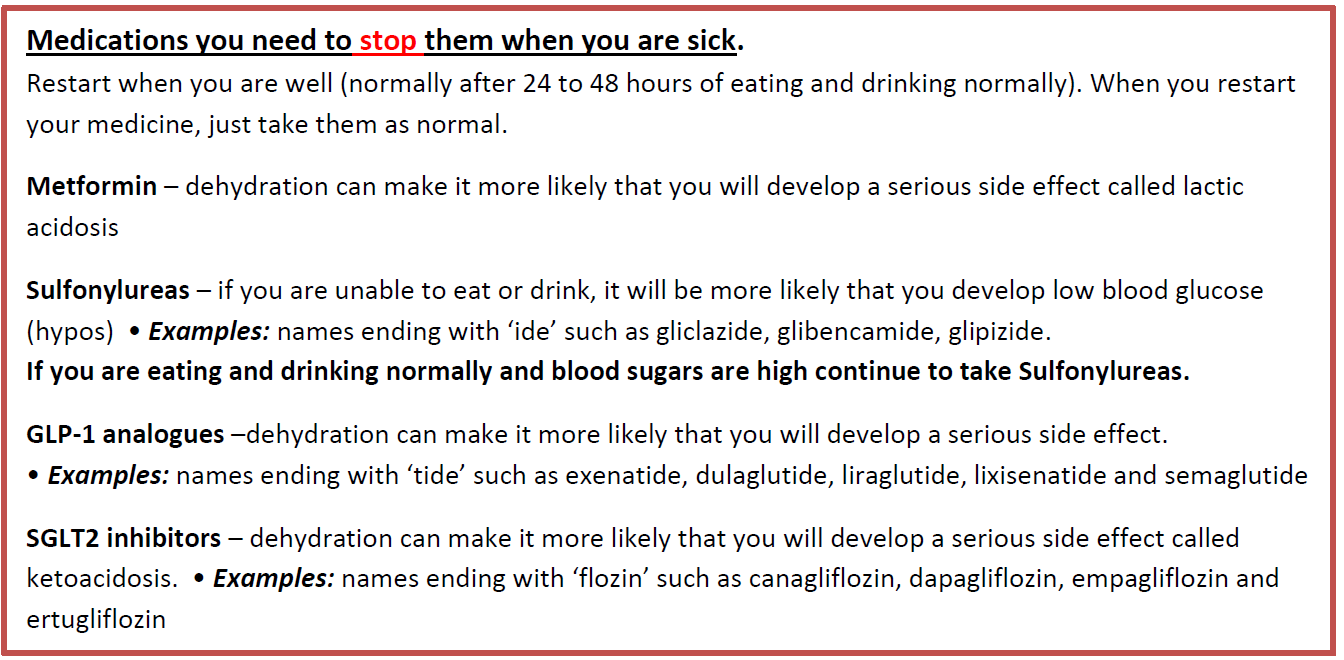
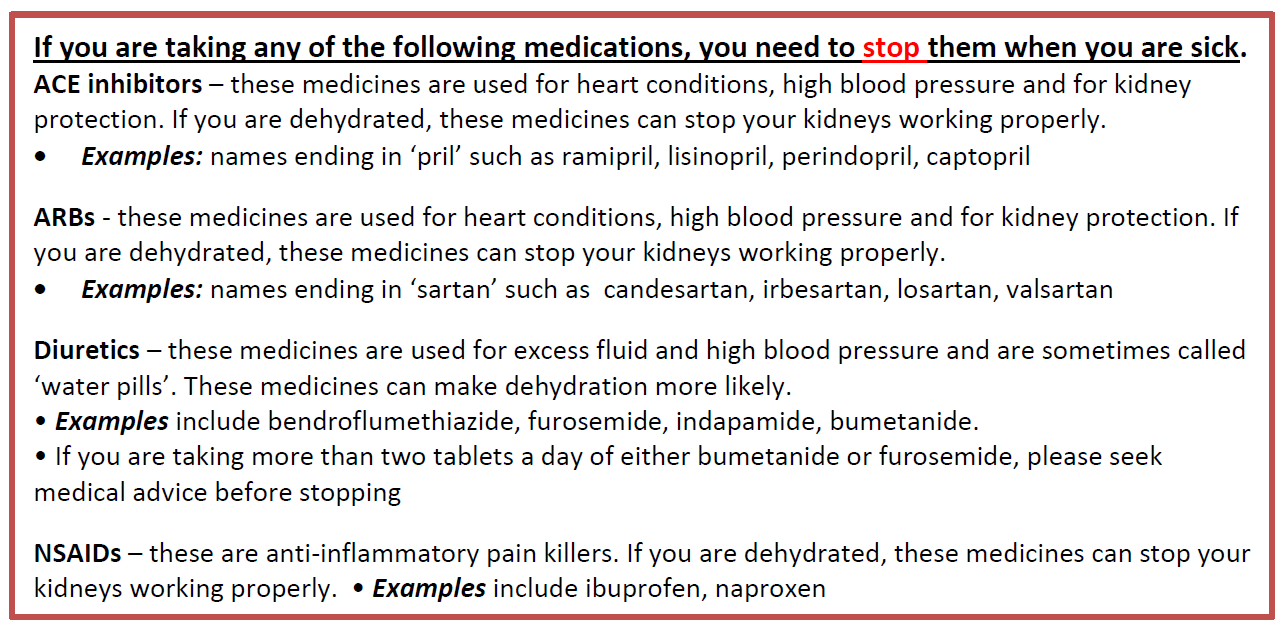
With respect to non-diabetic medications (5):
For those patients taking sulphonylurea medication:
- patients taking this medication should have access to blood glucose monitoring equipment; frequency of self-monitoring of blood glucose (SMBG) should be increased to a minimum of daily - with a range of fasting and pre-meals (especially if dietary intake is affected)
- appropriate advice should be provided regarding the increased risk of hypoglycaemia - usually more likely in the early stages of illness, especially if reduced dietary intake is a factor i.e. reinforce the importance of taking some form of regular carbohydrate
- the patient should be advised to contact their health care professional if glucose level increases beyond 17 mmol/L and/or the patient feels unwell, medical advice should be sought (2)
SGLT2 inhibitors and risk of diabetic ketoacidosis:
SGLT2 inhibitors increase the risk for diabetic ketoacidosis, particularly in patients with type 1 diabetes and those with certain high risk conditions
- in some cases blood glucose levels are normal or only mildly elevated, a condition known as euglycaemic ketoacidosis - this can delay the diagnosis
- it is advised to check ketones in patients taking SGLT2 inhibitors with symptoms or precipitating factors for ketoacidosis regardless of blood glucose levels (6)
In DKA associated with use of SGLT2 inhibitors:
- over a third of patients with ketoacidosis associated with SGLT2 inhibitor have normal or only mildly elevated blood glucose levels (<13.9 mmol/L, <250 mg/dL) - referred to as euglycaemic diabetic ketoacidosis (6)
- diagnosis can be delayed because of the absence of hyperglycaemia and the less severe polyuria polydipsia, owing to the milder degree of hyperglyacemia-induced osmotic diuresis
Possible predisposing conditions for the development of diabetic ketoacidosis in patients taking SGLT2 inhibitors include:
- excessive alcohol use or illicit drug use
- adherance to a very low carbohydrate or ketogenic diet
- unwillingness or inability to monitor ketone bodies
- pregnancy
- past history of diabetic ketoacidosis
- use of an insulin pump
- inappropriate reduction of insulin dose when using SGLT2 inhibitor
- late-onset autoimmune diabetes of adulthood (LADA)
Possible precipitating factors for diabetic ketoacidosis in patients taking SGLT2 inhibitors include:
- volume depletion/dehydration
- vomiting
- prolonged or vigorous exercise
- a failure of insulin pump or insulin infusion site
- acute illness
- hospitalisation for surgery
- travel where there has been a disruption of usual insulin regime
Information for healthcare professionals (7)
- rare cases of diabetic ketoacidosis, including life-threatening ones, have occurred in patients taking SGLT2 inhibitors, used to treat type 2 diabetes. A number of these cases were atypical with patients having only moderately raised blood sugar levels and some of them occurred during off-label use and clinical trials in patients with type 1 diabetes
- always consider the possibility of diabetic ketoacidosis in patients taking SGLT2 inhibitors who have non-specific symptoms such as nausea, vomiting, anorexia, abdominal pain, excessive thirst, difficulty breathing, confusion, unusual fatigue or sleepiness
- inform patients of the signs and symptoms of diabetic ketoacidosis and advise them to seek medical advice immediately if they develop such signs and symptoms
- stop treatment with SGLT2 inhibitors immediately if diabetic ketoacidosis is suspected or confirmed, and do not re-start treatment unless another clear precipitating factor for the condition is identified and resolved
- stop treatment with SGLT2 inhibitors temporarily in patients undergoing major surgical procedures or hospitalised due to acute serious medical illnesses. Treatment may be restarted once the patient's condition has stabilised
SGLT2 inhibitors: monitor ketones in blood during treatment interruption for surgical procedures or acute serious medical illness (8):
- SGLT2 inhibitor treatment should be interrupted in patients who are hospitalised for major surgical procedures or acute serious medical illnesses and ketone levels measured, preferably in blood rather than urine. Treatment may be restarted when the ketone values are normal and the patient's condition has stabilised
- Advice for healthcare professionals:
- interrupt sodium-glucose co-transporter 2 (SGLT2) inhibitor treatment in patients who are hospitalised for major surgical procedures or acute serious medical illnesses
- monitor ketones during this period – measurement of blood ketone levels is preferred to urine
- restart treatment with the SGLT2 inhibitor once ketone values are normal and the patient’s condition has stabilised
- report suspected adverse drug reactions to SGLT2 inhibitors to the Yellow Card Scheme
Diagnosis of diabetic ketoacidosis if on an SGLT2 inhibitor (6):
- because blood glucose levels are often lower in diabetic ketoacidosis associated with SGLT2 inhibitor use - euglycaemic diabetic ketoacidosis - then the omostic diuresis associated with diabetic ketoacidosis occuring in other circumstances is not always a prominent symptom
- if clinical features suggestive of possible diabetic ketoacidosis then
- increased ketones in blood (beta-hydroxybutyrate >= 3 mmol/L) or urine (ketonuria ++ or higher on urine dipsticks) - note that blood ketone testing is preferred over urine test strips as it is more accurate for detecting onset and resolution of ketosis
- acidosis—serum bicarbonate <15 mmol/L and/or blood pH <7.3
For those taking insulin therapy:
Encourage adequate dietary and fluid intake:
- Advice is similar to that for Type 2 Diabetes treated with oral sulphonylurea medication, with greater emphasis again on the importance of regular carbohydrate intake and options for lighter carbohydrate foodstuffs (especially at usual mealtimes/when insulin is administered)
Increase frequency of blood glucose monitoring/advice re insulin therapy:
- Frequency of SMBG should be increased to a minimum of twice a day - with a range of fasting and pre-meal testing (especially if dietary intake is affected)
- INSULIN SHOULD NEVER BE OMITTED, despite a reduction in dietary intake; often both patients and carers have to be convinced that this is the appropriate course of action
- Increased insulin requirements are often required during periods of illness and ill-health; the patient should be advised to contact their healthcare professional if blood glucose levels are persistently > 25 mmols/mol (3)
- It is appropriate to provide the patient with a simple and individualised plan for adjusting insulin based on blood glucose results
Admission or specialist advice in type 2 diabetes (3,4)
The decision to admit a person or seek specialist advice will depend on clinical judgement, taking into account the person's age, underlying comorbidities and complications, and the presence of hyperglycaemia and ketosis.
- immediate hospital admission is indicated if:
- is an immediate risk of diabetic ketoacidosis (DKA)
- blood glucose persistently >20 mmol/L despite best therapy (3)
- there is moderate ketonuria (2+ on urine dipstick) or ketonaemia (1.5–2.9 mmol/L) with or without hyperglycaemia and the person cannot eat or drink, as there is a risk of DKA
- a person treated with insulin does not improve rapidly with insulin treatment (4)
- consider arranging hospital admission or seeking urgent specialist advice if (4):
- underlying condition is unclear
- person is dehydrated or at risk of dehydration
- vomiting persists beyond 2 hours.
- person and their family/carers are unable to keep the blood glucose level above 3.5 mmol/L.
- person and their family/carers are exhausted, for example due to repeated night-time waking.
Reference:
- Down S. How to advise on sick day rules. Diabetes & Primary Care (2018); 20 (1): 15-16.
- NHS London Clinical Networks. Sick day rules: how to manage Type 2 diabetes if you become unwell with coronavirus and what to do with your medication (Accessed 8/5/2020)
- Patient.co.uk (Accessed 8/5/2020).Diabetes and Intercurrent Illness.
- CKS (Accessed 8/5/2020). Type 2 Diabetes.
- NHS Sandwell and West Birmingham CCG (Accessed 23/9/2020). Sick day rules: how to manage Type 2 diabetes if you become unwell with coronavirus and what to do with your medication
- Musso G et al. Diabetic ketoacidosis with SGLT2 inhibitors.BMJ 2020;371:m4147 http://dx.doi.org/10.1136/bmj.m4147
- EMA (16/2/16).EMA confirms recommendations to minimise ketoacidosis risk with SGLT2 inhibitors for diabetes
- MRHA (18/3/2020). SGLT2 inhibitors: monitor ketones in blood during treatment interruption for surgical procedures or acute serious medical illness
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.