Vulvodynia
- Vulvodynia
- term used to describe unexplained vulvar pain, sexual dysfunction, and resultant psychological disability (1,2)
- is chronic vulval pain lasting more than three months without an identifiable cause, and is classified as primary (present from the first physical contact) or secondary (arising after an initial pain-free period) (3)
- summary features (4)
- if there is a present cause for the condition (lichen sclerosis, inflammation, etc.), this is not a case of vulvodynia
- symptoms may be described as itching, burning, stinging, irritation, stabbing, and/or rawness
- classification of vulvodynia is based on the description of the pain itself
- symptoms may involve the whole vulva (generalised vulvodynia) or may be localised in certain portions of the genitalia such as the clitoris (clitorodynia) or the vestibule of the vagina (vestibulodynia)
- depending on whether there is a provoking aspect or not, the vulvodynia may be provoked vulvodynia (caused by placement of a swab, sexual intercourse), unprovoked vulvodynia (if there is no provoking aspect), or mixed
- may be divided into intermittent, persistent, constant, immediate, or delayed
- some patients experience allodynia (defined as pain resulting from stimuli which would not normally cause pain), such as touch or pressure
- incidence of vulvodynia may be more than 15% among patients attending gynecology clinics
- Investigation and diagnosis:
- evaluation of the patient with vulvodynia should include detailed medical and sexual history, systemic and pelvic examination, microbiologic cultures, colposcopy and biopsy if it is necessary
- diagnosis of vulvodynia is made based on the principle of exclusion (4)
- exclusion of all other treatable causes before making a diagnosis of vulvodynia is obligatory
- detailed medical history is necessary based on patient-reported written data, which includes the duration of pain syndrome, detailed history of the medical condition, sexual history, allergies, and previous treatment
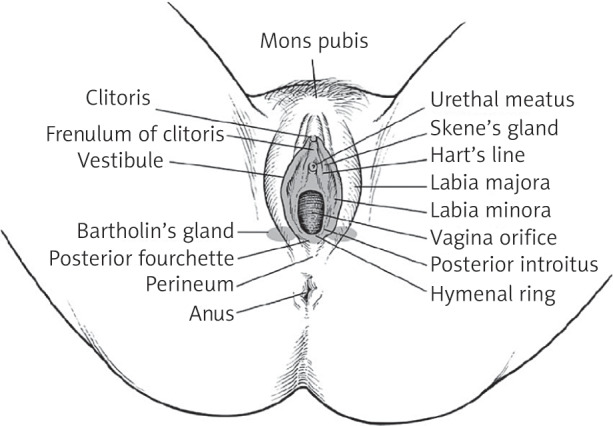
- a good knowledge of vulvar anatomy is of exceptional significance for making of the diagnosis
- diagnosis of vulvodynia is made based on the principle of exclusion (4)
- evaluation of the patient with vulvodynia should include detailed medical and sexual history, systemic and pelvic examination, microbiologic cultures, colposcopy and biopsy if it is necessary
- cotton swab testing is used in order to identify the zones of pain
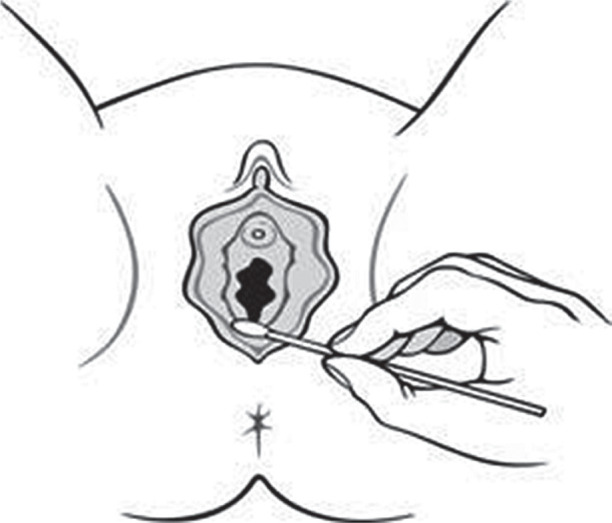
- using a cotton swab, demonstrate, in a neutral area (e.g, the inner thigh), that you will be pressing it gently on various points of the vulva (3)
- ask the patient to rate their pain on a scale of 0-10 with 0 being no pain and 10 being the worst possible pain
- is also to differentiatiate between localised and generalised forms of the condition
- vulva and vagina must be examined thoroughly
- presence of vulvovaginal infection must be ruled out, when it is necessary
- when undertaking examination, a low-osmolarity, pH balanced lubricants are preferred to minimise discomfort and protect the vaginal epithelium (3)
- vulvar pain may also be reflected pain from other parts of the body, such as the back or flanks, so musculoskeletal evaluation should be considered
- musculoskeletal assessment would help in ruling out of factors associated with vulvodynia such as pelvic muscular hyperactivity and myofascial or other biomechanical disorder
- a narrow or tight vaginal introitus typically reflects increased tone of the levator ani muscles, whereas a more compliant and flexible opening is palpated when these muscles are relaxed (3)
- the most effective palpation of the obturator internus muscle is while the patient actively abducts the thigh, which increases tension in the muscle
- when the patient relaxes the leg, the muscle softens, allowing clearer assessment of its baseline tone
- the most effective palpation of the obturator internus muscle is while the patient actively abducts the thigh, which increases tension in the muscle
- a narrow or tight vaginal introitus typically reflects increased tone of the levator ani muscles, whereas a more compliant and flexible opening is palpated when these muscles are relaxed (3)
- Treatment
- general measures in management of vulvodynia
- taking measures for delicate genital hygiene is necessary (4)
- use of non-irritating, cotton underwear, avoiding of the use of vulvar irritating agents (perfumes, shampoos, showers), and use of soft, non-irritating soaps
- it is possible for the vulva to be cleaned only with clean water and subsequent use of a moisture-preserving emollient in the involved area in order to prevent excessive drying and to act as a barrier function
- during menstruation the usage of delicate cotton sanitary pads is strongly recommended
- good drying and cleaning of the vulva is necessary after urination
- good lubrication with non-irritating agents is recommendable for sexual intercourse
- use of non-irritating, cotton underwear, avoiding of the use of vulvar irritating agents (perfumes, shampoos, showers), and use of soft, non-irritating soaps
- taking measures for delicate genital hygiene is necessary (4)
- manage any identified pathologies related to vulval pain in line with local protocols and guidelines (3)
- for example granulation tissue can cause vulval pain and may occur as part of the healing process in perineal or vaginal tears postpartum
- if granulation tissue is found on examination, then the granulation tissue can be cauterised with silver nitrate to treat associated vulval pain
- topical oestrogen alone can be used in cases of genitourinary syndrome of menopause
- for example granulation tissue can cause vulval pain and may occur as part of the healing process in perineal or vaginal tears postpartum
- idiopathic vulvodynia
- treatment of vulvodynia is individualised and multimodal, including lifestyle modifications, psychotherapy, psychosexual counselling, pelvic floor physiotherapy, medications, and rarely, surgical interventions (3)
- physical therapy (4)
- includes assessment of the patient’s pelvic muscles, joints, fasciae, and ligaments
- assessment of the adjacent pelvic organs – urinary bladder, large intestine – is also necessary
- most of the therapies include weekly sessions of one or two hours, which are focused most frequently on training of the muscles of the pelvic fundus, soft tissue mobilisation, joint manipulation, muscle relaxation, and general tone balance
- topical preparations
- most commonly used local medication is lidocaine ointment 5%, which is used 30 minutes before sex or when the patient has complaints (4)
- male sexual partners may experience penile numbness and should avoid oral contact
- a review however notes (3) "..Based on our experience of patients’ disclosures, temporary pain reduction can facilitate intercourse for a partner’s benefit rather than promote symptom improvement for the patient. Furthermore, patients may dislike the sensation of their skin being numb, particularly during penetrative intercourse. When patients decide to use lidocaine for temporary symptom relief, counsel them that skin sensitivity may develop following use.."
- most commonly used local medication is lidocaine ointment 5%, which is used 30 minutes before sex or when the patient has complaints (4)
- electrical stimulation
- an emerging treatment for vulvodynia is transcutaneous electrical nerve stimulation (4)
- tricyclic antidepressants and other drugs used to treat neuropathic pain are sometimes useful as an adjunct to treatment with biofeedback
- surgery
- when a series of non-surgical methods have been tried and failed, and the pain has been localised in the vestibule, vestibulectomy may be an effective treatment (4)
- represents an excision in the region of the painful part of vestibule to the lateral vestibular walls at Hart’s line, including all tender parts extending to the anterior vestibule, if necessar
- when a series of non-surgical methods have been tried and failed, and the pain has been localised in the vestibule, vestibulectomy may be an effective treatment (4)
- general measures in management of vulvodynia
Reference:
- Paavonen J. Vulvodynia—a complex syndrome of vulvar pain, Acta Obstet Gynecol Scand 1995;74: 243–247.
- Glazer HI, Ledger WJ. Review clinical management of vulvodynia. Rev Gynaecol Pract 2002;2: 83–90.
- Braunstein M et al. Vulvodynia (chronic vulval pain).BMJ 2026; 392.
- Vasileva P, Strashilov SA, Yordanov AD. Aetiology, diagnosis, and clinical management of vulvodynia. Prz Menopauzalny. 2020 Mar;19(1):44-48.0(4):283-90.
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page