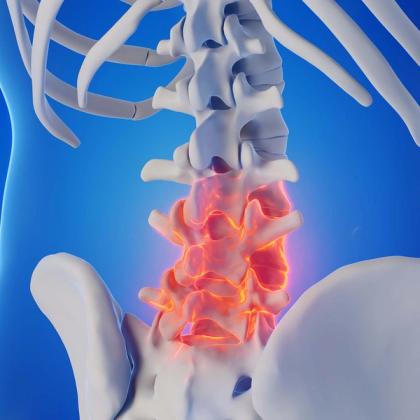
Ankylosing spondylitis (AS) is a chronic, immune-mediated inflammatory disorder that predominantly targets the axial skeleton, especially the spine and sacroiliac joints. This condition evolves insidiously, often beginning in young adulthood, and gradually imposes limitations on spinal mobility, eventually leading to fusion in advanced cases. Beyond its skeletal manifestations, AS can also extend its reach to various extra-articular organs, emphasising the systemic nature of the disease. In this episode, Dr Roger Henderson looks at its clinical presentation, how to diagnose it, the treatment options available and its prognosis.
Key take-home points
- AS typically presents before the age of 40, with the majority of affected individuals experiencing initial symptoms during their late teens to early thirties.
- HLA-B27 is present in about 90% of patients who have AS, but its role in the pathogenesis of AS remains unclear.
- The underlying pathophysiology of AS involves chronic inflammation at sites where ligaments, tendons and joint capsules attach to bone – regions referred to as entheses. This process, termed enthesitis, is central to the disease mechanism and distinguishes AS from many other forms of inflammatory arthritis.
- Clinically, the hallmark of AS is persistent back pain that demonstrates inflammatory characteristics. Morning stiffness lasting more than 30 minutes and nocturnal pain that disturbs sleep and improves upon getting out of bed are also common.
- Over time, progressive spinal rigidity can lead to postural deformities.
- Extra-articular manifestations include anterior uveitis (which can affect as many as one-third of patients), inflammatory bowel disease and psoriasis.
- Diagnosing AS requires a combination of clinical, imaging and laboratory findings, although there is no specific test.
- Inflammatory markers such as erythrocyte sedimentation rate and C-reactive protein are elevated in the majority of active cases but may remain normal in a substantial subset.
- Testing for HLA-B27 can provide supportive evidence, especially in equivocal cases, but should not be used in isolation to confirm or exclude the diagnosis.
- Imaging studies play a key role in both diagnosis and disease monitoring, and plain radiographs remain the initial modality of choice.
- Non-steroidal anti-inflammatory drugs (NSAIDs) remain the first-line drug treatment option in AS.
- Oral steroids are not recommended in AS due to limited efficacy in axial disease.
- Tumour necrosis factor inhibitors (TNFi) are options for severe active AS in adults whose disease has responded inadequately to, or patients who cannot tolerate, NSAIDs.
- Interleukin-17 inhibitors (IL-17i) may be considered in patients unresponsive to TNFi or in those with coexisting psoriasis.
- Janus kinase inhibitors can be considered for patients with AS who are unresponsive or have contraindications to both TNFi and IL-17i.
- If left untreated, AS can cause significant spinal deformities, with around one-third of AS patients eventually suffering from a thoracolumbar kyphosis.
- Cardiovascular disease is the leading cause of death in patients with AS.
Key references
- NICE. 2017. https://www.nice.org.uk/guidance/ng65.
- Wenker KJ, Quint JM.In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.
- Kim SH, Lee S-H. J Rheum Dis. 2023;30(4):220-233. doi: 10.4078/jrd.2023.0041.
- Kroon FPB, et al. J Rheumatol. 2016;43(3):607-617. doi: 10.3899/jrheum.150721.
- van der Heijde D, et al. Ann Rheum Dis. 2017;76(6):978-991. doi: 10.1136/annrheumdis-2016-210770.
- NICE. 2016. https://www.nice.org.uk/guidance/ta383/chapter/1-recommendations.
- Zhu W, et al. Bone Res. 2019:7:22. doi: 10.1038/s41413-019-0057-8. eCollection 2019.
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page