Primary hyperparathyroidism is the most common cause of hypercalcaemia. Diagnosis of hypercalcaemia is made by measuring the total serum calcium.
- prolonged application of a tourniquet when taking blood should be avoided since it is thought to increase the calcium levels
- circulating calcium contains both the free and albumin-bound components. Around 45% of serum calcium is bound to albumin hence following calculation is used to calculate the adjusted calcium levels
- corrected calcium=measured calcium+(40-measured albumin)×0.02, where calcium concentrations are in mmol/L and albumin is in g/L.
- this formula helps in excluding factitious causes of hypercalcaemia
- repeat the test to confirm (unless patient acutely unwell ot symptomatic in which case immediate referral should be considered)
- hypercalacemia can be
- mild hypercalcaemia - adjusted calcium concentration is 2.65–3.00 mmol/L
- moderate hypercalcaemia - adjusted calcium concentration is 3.01–3.40 mmol/L
- severe hypercalcaemia - adjusted calcium concentration is more than 3.40 mmol/L
Although not carried out routinely in primary care setting, increased ionized calcium levels also helps in excluding factitious causes of hypercalcaemia
Measurement of PTH is the next step in the evaluation of hypercalcaemia.
- raised level of intact PTH (or a level that is in an unexpected “normal” range) simultaneous with an elevated calcium level generally indicates a diagnosis of primary hyperparathyroidism
- similar picture may be seen in lithium or thiazide use, tertiary hyperparathyroidism associated with end-stage renal failure, and familial hypocalciuric hypercalcaemia)
- normal level of corrected or ionized serum calcium and an elevated level of PTH in patients with no other causes of secondary hyperparathyroidism is consistent with normocalcemic primary hyperparathyroidism.
Other associated laboratory findings in primary hyperparathyroidism include:
- serum phosphate:
- decreased in about half of cases
- a raised serum phosphate suggests nonparathyroid hypercalcaemia
- a normal serum phosphate is not diagnostically useful
- urine Ca - increased in most patients
- metabolic acidosis is reflected by reduced plasma bicarbonate and high plasma chloride
The main goal of further laboratory investigations are to find and rule out other causes of hypercalcaemia. Some of the investigations carried out include
- urinary calcium to creatinine clearance ratio
- helps distinguish between primary hyperparathyroidism (calcium to creatinine clearance ratio is greater than 0.01) and familial hypocalciuric hypercalcaemia (less than 0.01 in about 80% of patients),
- assessment of renal function and the level of serum 25-hydroxyvitamin D
- renal ultrasonography
- dual-energy x-ray absorptiometry (DEXA) - for screening and monitoring of osteopenia and osteoporosis
- parathyroid imaging – used for operative planning (3)
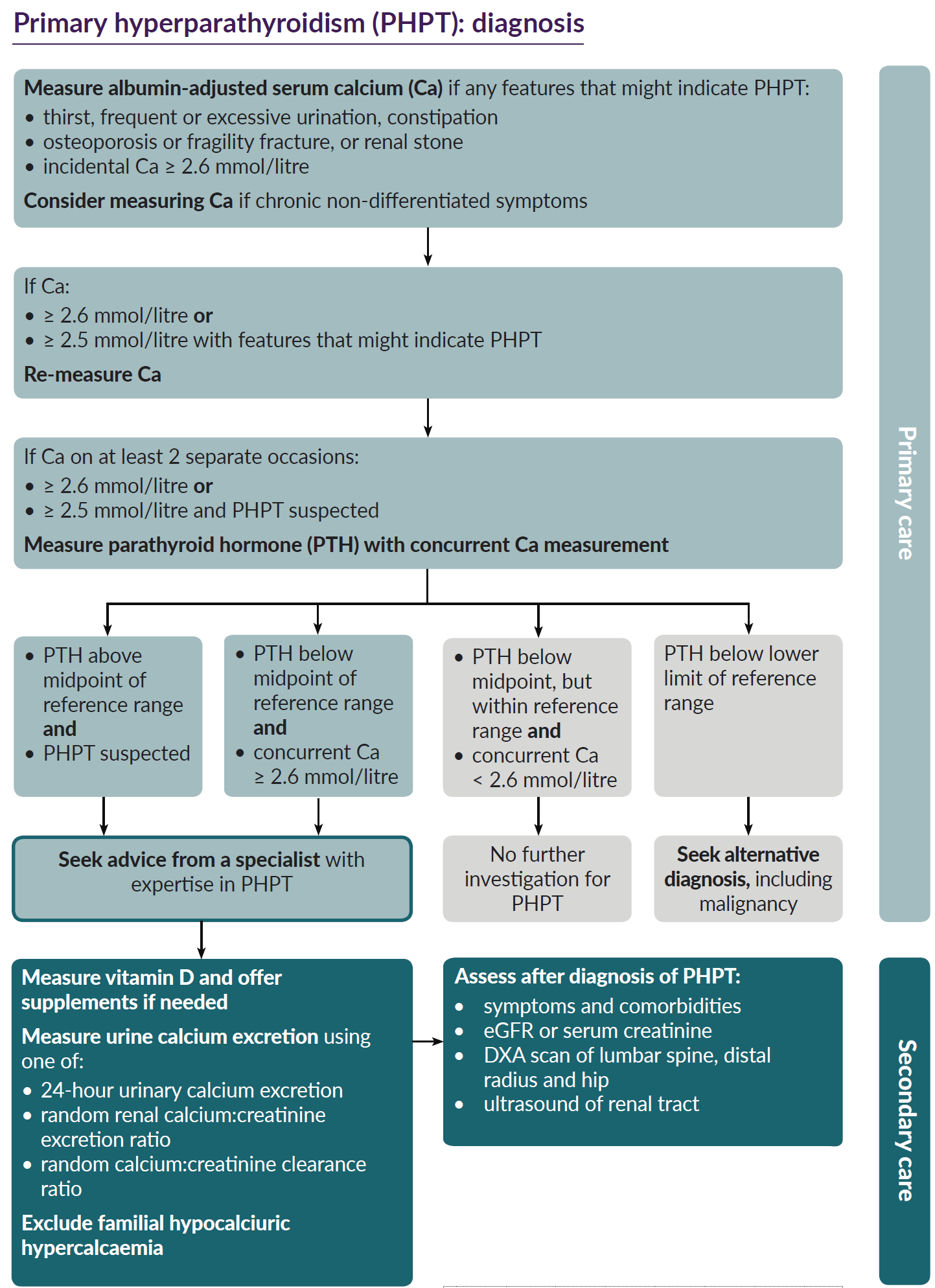
NICE have suggested a schemata for the diagnosis of primary hyperparathyroidism in primary care (4):
Note:
- primary hyperparathyroidism can also exist concomitantly with a tumour,
Reference:
- (1) Smellie WS et al. Best practice in primary care pathology: review 11. J Clin Pathol. 2008 Apr;61(4):410-8.
- (2) Pallan S, Rahman MO, Khan AA. Diagnosis and management of primary hyperparathyroidism. BMJ. 2012;344:e1013
- (3) AACE/AAES Task Force on Primary Hyperparathyroidism.The American Association of Clinical Endocrinologists and the American Association of Endocrine Surgeons position statement on the diagnosis and management of primary hyperparathyroidism. Endocr Pract. 2005;11(1):49-54
- (4) NICE (May 2019). Primary Hyperparathyroidism.
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page