Start blind and refine as the identity of the underlying agent becomes more certain. Note any previously administered antibiotics which may obscure findings.
With respect to management in the community (1):
- chest Xray
- it is not necessary to perform a chest radiograph in patients with suspected community acquired pneumonia (CAP) unless:
- the diagnosis is in doubt and a chest radiograph will help in a differential diagnosis and management of the acute illness
- progress following treatment for suspected CAP is not satisfactory at review
- the patient is considered at risk of underlying lung pathology such as lung cancer
- it is not necessary to perform a chest radiograph in patients with suspected community acquired pneumonia (CAP) unless:
- general investigations are not necessary for the majority of patients with CAP who are managed in the community. [C] Pulse oximeters allow for simple assessment of oxygenation. General practitioners, particularly those working in out-of-hours and emergency assessment centres, should consider their use
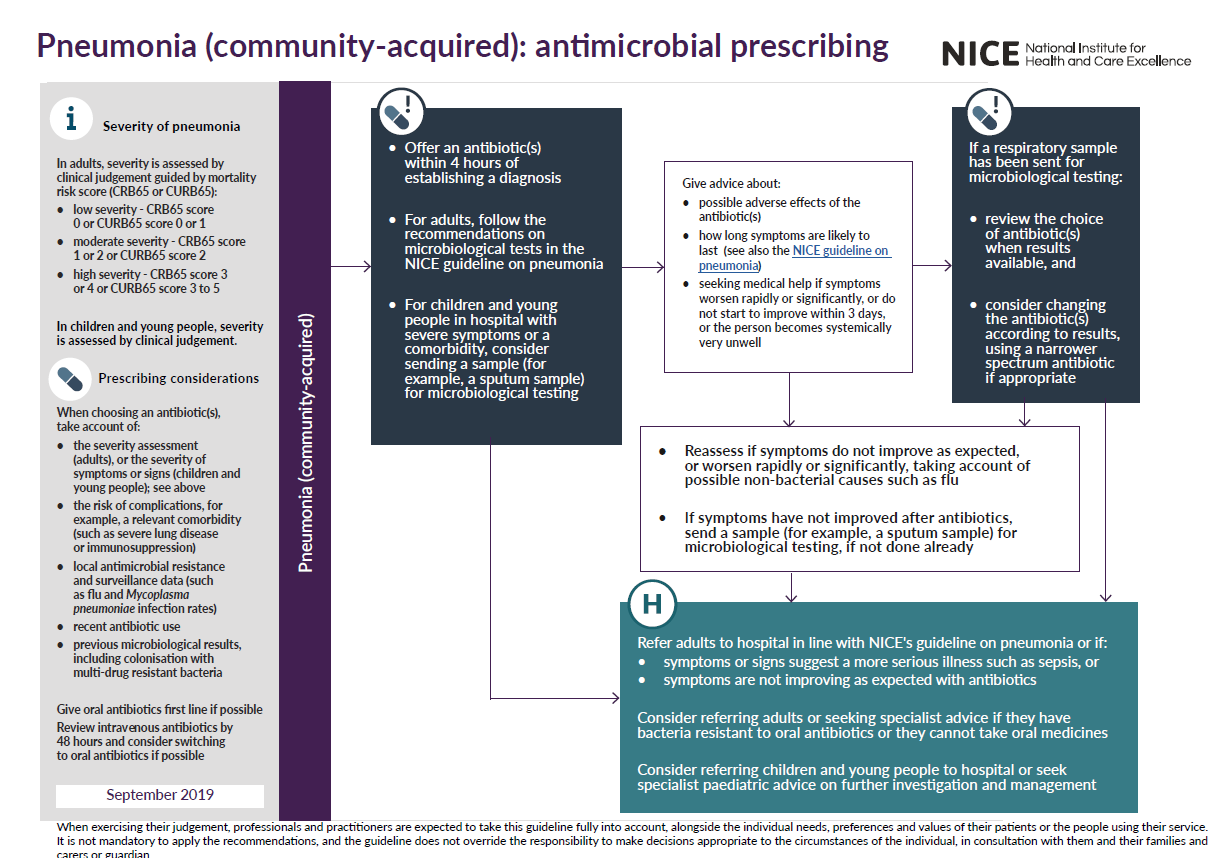
NICE suggest (3,4):
With respect to hospital:
- First, collect sputum and blood and send for gram stain and culture. Order a chest X-ray and more specialist investigations according to suspicions.
Community acquired pneumonia:
- Initial Empirical therapy for CAP in Adults (1,2,3,4):
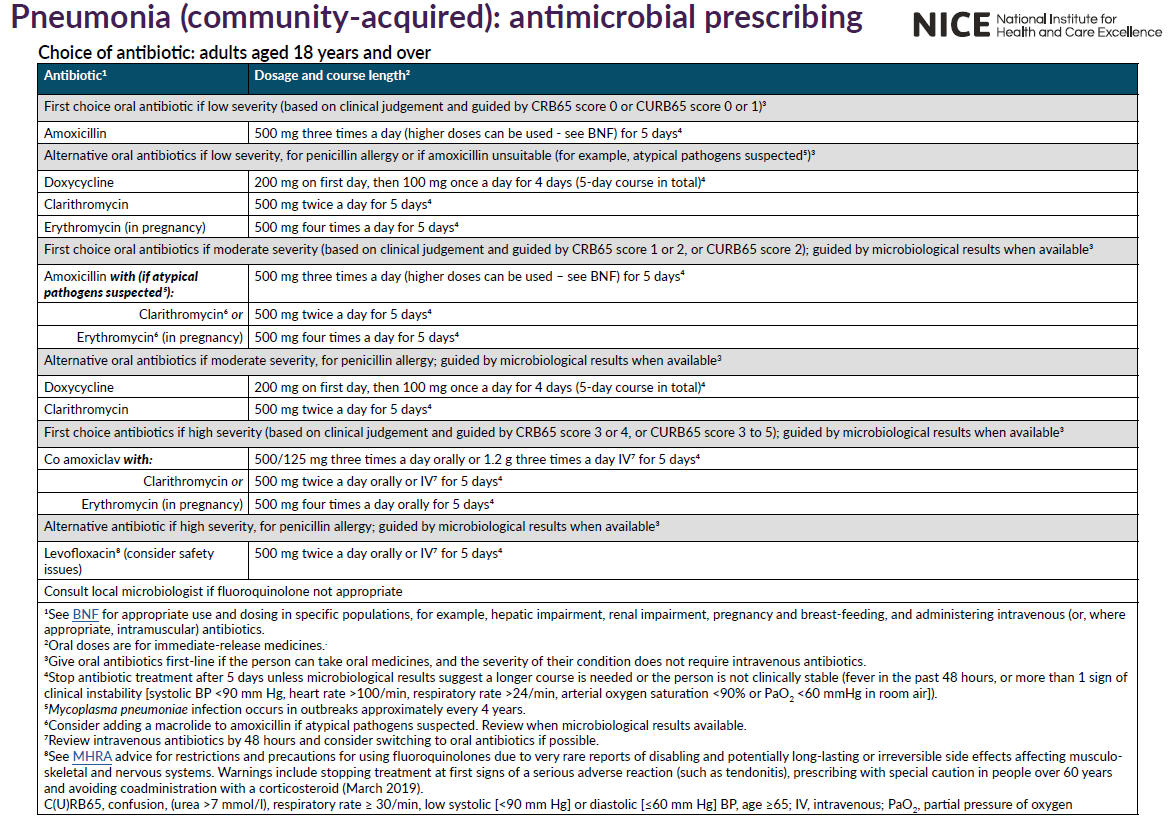
- uncomplicated community-acquired pneumonia:
- amoxicillin remains the first choice in the UK - if the patient is treated at home (not severe) then the dose of amoxicillin is 500mg-1g tds* PO (1)
- in patients allergic to penicillin, a suitable alternative is clarithromycin 500mg bd PO (1)
- if atypical pneumonia is suspected then add erythromycin or another macrolide (e.g. azithromycin or clarithromycin); if staphylococcus is suspected e.g. in influenza or measles, then add flucloxacillin
- * BTS guidelines recommend adequate dosing of amoxicillin to cover intermediate-resistant strains of Strep pneumoniae
- stop antibiotic treatment after 5 days unless microbiological results suggest a longer course is needed or the person is not clinically stable (fever in the past 48 hours, or more than 1 sign of clinical instability [systolic BP <90 mm Hg, heart rate >100/min, respiratory rate >24/min, arterial oxygen saturation <90% or PaO2 <60 mmHg in room air]) (4)
- amoxicillin remains the first choice in the UK - if the patient is treated at home (not severe) then the dose of amoxicillin is 500mg-1g tds* PO (1)
- pneumonia possibly caused by atypical pathogens
- erythromycin
- severe Legionella infections may require the addition of rifampicin; tetracycline is an alternative for mycoplasma and chlamydial infections; treatment is for at least 14 days (14-21 days for Legionella)
- erythromycin
Hospital acquired:
A broad-spectrum cephalosproin (e.g. cefotaxime or ceftazidime) or an antipseudomonal penicillin or another antipseudomonal beta-lactam. Metronidazole will be required if anaerobe infection. Immunosuppressed patients may require high dose broad spectrum antibiotics, antifungal and antiviral agents.
Reference:
- 2015 - Annotated BTS Guideline for the management of CAP in adults (2009) Summary of recommendations.
- Hoare Z, Lim WS.Pneumonia: update on diagnosis and management. BMJ. 2006 May 6;332(7549):1077-9
- NICE (December 2014).Pneumonia- Diagnosis and management of community- and hospital-acquired pneumonia in adults
- NICE (September 2019). Pneumonia (community-acquired): antimicrobial prescribing
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page