Exoerythrocytic schizogony in malaria
Last reviewed dd mmm yyyy. Last edited dd mmm yyyy
transmission
Malaria is a parasitic disease caused by genus Plasmodium. The parasite is spread by female Anopheles mosquitoes and five species of Plasmodium regularly infect humans:
- P. falciparum - most dangerous form, accountable for majority of deaths throughout the world
- P. ovale - a relapsing malaria
- P. vivax - a relapsing malaria
- P. malariae - least common type present in UK, may present with late recrudescence after many years
- Plasmodium knowlesi - very rarely imported at present, but capable of producing severe illness
Anopheles mosquitoes exclusively transmit malaria from one person to another.
- around 20 different Anopheles species are locally important around the world
- Anopheles mosquitoes breed in water and each species has its own breeding preference e.g. -some prefer shallow collections of fresh water, such as puddles, rice fields, and hoof prints
Intensity of transmission may vary with factors related to:
- the parasite
- the vector
- transmission is more intense in places where the mosquito lifespan is longer (so that the parasite has time to complete its development inside the mosquito) and where it prefers to bite humans rather than other animals e.g - the long lifespan and strong human-biting habit of the African vector species is the main reason why about 90% of the world's malaria deaths are in Africa
- transmission is more intense in places where the mosquito lifespan is longer (so that the parasite has time to complete its development inside the mosquito) and where it prefers to bite humans rather than other animals e.g - the long lifespan and strong human-biting habit of the African vector species is the main reason why about 90% of the world's malaria deaths are in Africa
- the human host
- human immunity especially among adults in areas of moderate or intense transmission conditions
- although partial immunity will not provide complete protection it will reduce the risk of causing severe disease
- the environment
- rainfall patterns, temperature and humidity which affects the number and survival of mosquitoes
- malaria transmission is seasonal, with the peak during and just after the rainy season.
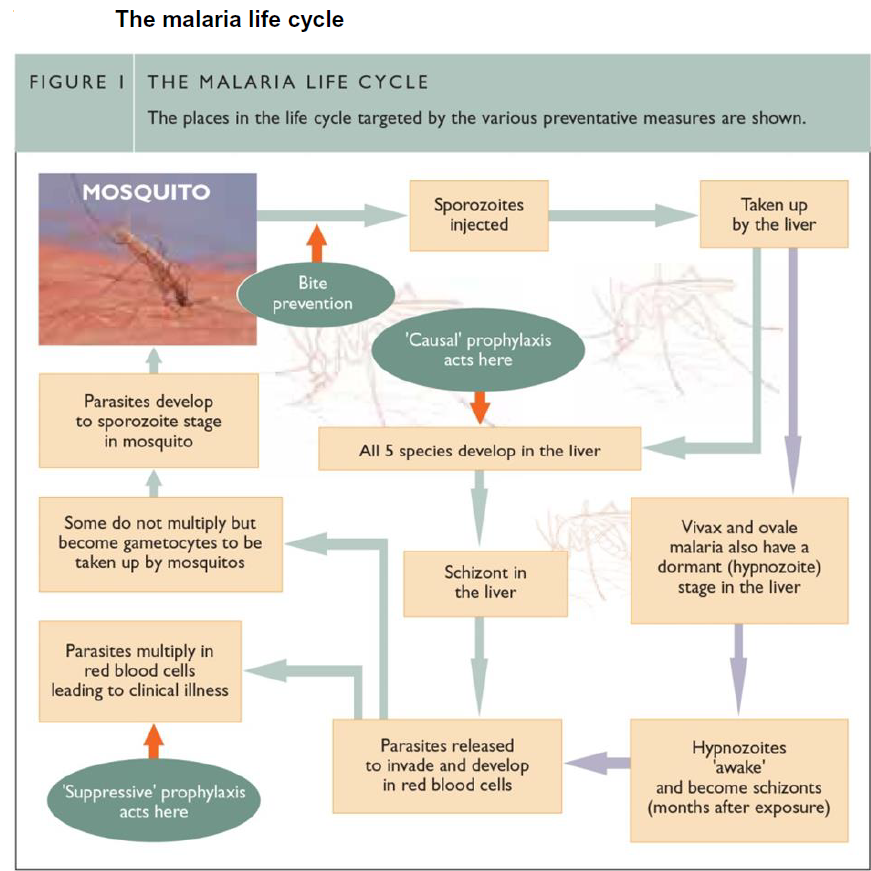
Humans, who are the intermediate hosts, become infected by the bite of an infected female Anopheles mosquito.
- the mosquito injects around 10-15 sporozoites (the infecting agent) in to the blood circulation which circulates and enters liver cells
- theses sporozoites divide inside liver cells into a schizont containing approximately 30,000 offspring (merozoites) which are released into the bloodstream when the schizont ruptures
- vivax and ovale malaria also have a dormant (hypnozoite) stage in the liver which may ‘awake’ and become schizont (month after exposure)
- merozoites invades erythrocytes, grows and divides inside them over 24 hours (P.knowlesi), 48 hours (P. falciparum, vivax or ovale) or 72 hours (P. malariae) to form between 8 and 32 parasites, whereupon the red cell bursts to release them to infect new red cells
- these cycles in the red cells continue, increasing the numbers of parasites in the infected person and this asexual erythrocytic stage is responsible for the clinical symptoms of the disease (3)
- some merozoites develop into gametocytes (sexual stages) which may stay in circulation for several weeks. These gametocytes are taken up by the biting mosquitos where sexual reproduction occurs leading to formation of new infectious sporozoites inside mosquitos (thus completing the life cycle) (2,3)
The parasite can also be transmitted by blood transfusion, transplacentally, organ transplantation and via the use of improperly cleaned syringes (4).
Phases of malaria infection:
pre-erythrocyte schizogony
- this phase of malaria occurs after the introduction of sporozoites, the infective form of the parasite, through the skin by the Anopheles mosquito. In this phase the patient is asymptomatic and the patient is not infective. Sporozites that are not removed by the body's defences migrate to the liver and undergo development.
- after a variable period the micromerozoites are liberated. Sporozoites of P. vivax and P. ovale may remain in the liver in the form of hypnozoites
erythrocytic schizogony
- in this phase the red blood cells become infected by the micromerozoites. While in the red blood cells the micromerozoites pass through several stages of develop until they finally develop into merozoites. This asexual parasitic form is present at a variable time from when the human was inoculated with the sporozoite. In P.vivax this occurs at about 12 days, in P. falciparum about 9 days
- the red blood cells that are invaded is dependent on which form of Plasmodium the patient has been inoculated with. P. falciparum invades all red blood cells. P. vivax and P. ovale preferentially invade young red blood cells and reticulocytes. P. malariae preferentially invades senescent red blood cells. The merozoites then go through a cycle of where they pass through the various stages of development to produce more merozoites. As each cycle terminates the red cells are ruptured and the merozoite are released into the circulation
- the merozoites then may invade more red blood cells and the cycle continues again. The cycle occurs approximately every 48 hours in P. falciparum infection, every 48-72 hours in P. vivax
and P. ovale, and every 72 hours in P. malariae infection
gametogony
- gametogony occurs when a few merozoites develop into the sexual form of the parasite known as gametocytes. This may occur after the erythrocytic phase has been occurring for a considerable length of time
- once gametocytes are formed then the patient is infective. Only the mature forms of the gametocytes are found in the peripheral blood
exoerythrocytic schizogony (hypnozoite)
- this stage occurs with P. vivax and P. ovale where the parasites remain in a latent form in the liver
- P. malariae also has a latent form which remains in the blood
- in these benign forms of malaria relapse may therefore occur
- P. falciparum, does not have a latent form, and following successful cure no relapses occur.
Reference:
- (1) World Health Organization (WHO) 2014. Fact sheet. Malaria
- (2) Public Health England. Guidelines for malaria prevention in travellers from the UK 2019
- (3) Rosenthal PJ. Artesunate for the Treatment of Severe Falciparum Malaria. NEJM 2008; 358:1829-1836
- (4) Centers for disease control and prevention. Traveler's health - Yellow book
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page