Target blood pressure (BP ) levels
BP targets
- NICE suggest (1):
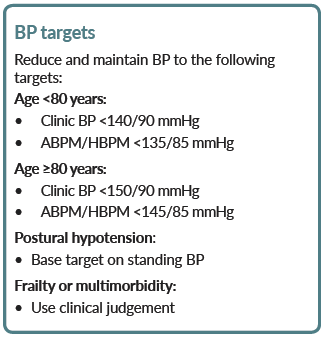
- NICE suggest target blood pressure levels in people with CKD:
- in people with CKD aim to keep the systolic blood pressure below 140 mmHg (target range 120-139 mmHg) and the diastolic blood pressure below 90 mmHg
- in people with CKD and diabetes, and also in people with an ACR of 70 mg/mmol or more, aim to keep the systolic blood pressure below 130 mmHg (target range 120-129 mmHg) and the diastolic blood pressure below 80 mmHg
- patients who are at the highest baseline risk of CVD have the most to gain from lowering of BP. Although it may not be possible to achieve target in all patients, any lowering of BP is beneficial. Aim to achieve the largest reduction possible towards the target, taking into account tolerability and concordance for each individual patients
Continuing treatment
- provide an annual review of care to monitor blood pressure, provide patients with support and discuss their lifestyle, symptoms and medication
- patients may become motivated to make lifestyle changes and want to stop using antihypertensive drugs. If at low cardiovascular risk and with well controlled blood pressure, these patients should be offered a trial reduction or withdrawal of therapy with appropriate lifestyle guidance and ongoing review
Please consult the complete guideline for more detailed advice
Blood pressure management and ICH (intracerebral haemorrhage) (2)
- consider rapid blood pressure lowering for people with acute intracerebral haemorrhage who do not have any of the exclusions * and who:
- present within 6 hours of symptom onset and
- have a systolic blood pressure of between 150 and 220 mmHg
- taking into account the risk of harm, consider rapid blood pressure lowering on a case-by-case basis for people with acute intracerebral haemorrhage who do not have any of the exclusions listed * and who:
- present beyond 6 hours of symptom onset or
- have a systolic blood pressure greater than 220 mmHg
- when rapidly lowering blood pressure in people with acute intracerebral haemorrhage, aim to reach a systolic blood pressure of 140 mmHg or lower while ensuring that the magnitude drop does not exceed 60 mmHg within 1 hour of starting treatment
- when considering blood pressure lowering in young people aged 16 or 17 with acute intracerebral haemorrhage who do not have any of the exclusions listed*, seek advice from a paediatric specialist
- * exclusions:
- do not offer rapid blood pressure lowering to people who:
- have an underlying structural cause (for example, tumour, arteriovenous malformation or aneurysm)
- have a score on the Glasgow Coma Scale of below 6
- are going to have early neurosurgery to evacuate the haematoma
- have a massive haematoma with a poor expected prognosis
- do not offer rapid blood pressure lowering to people who:
- the NICE committee noted:
- committee decided to remove the aim of reaching the target within 1 hour because only a minority (33.4%) of participants in the INTERACT2 trial achieved the target of 140 mmHg within 1 hour and, more importantly, to avoid the potential harm of reducing systolic blood pressure by more than 60 mmHg in the first hour
- was evidence that rapidly lowering blood pressure does not increase the risk of neurological deterioration caused by reduced blood flow to the brain and has the potential to improve quality of life
- agreed that while there is some evidence that rapid blood pressure lowering treatment is beneficial, there may be an increase in adverse renal events, and they were concerned about the lack of evidence in people who are frail
- evidence that a moderate reduction of up to 60 mmHg within the first hour was associated with better outcomes such as functional independence
- a reduction of more than 60 mmHg within 1 hour was associated with significantly worse outcomes such as renal failure, early neurological deterioration, and death, compared with standard treatment
- therefore, the committee agreed that a large reduction of 60 mmHg or more within 1 hour should be avoided
Notes:
- The American college of cardiology has recommended BP thresholds for initiating antihypertensive treatment in patients with following medical conditions (3):
| BP threshold (to initiate treatment) mmHg | BP goal (mmHg) |
general | ||
clinical CVD or 10-year atherosclerotic cardiovascular disease (ASCVD) risk >=10% | >=130/80 | <130/80 |
no clinical CVD and 10 year ASCVD risk <10% | >=140/90 | <130/80 |
older persons ( >=65 years of age; non-institutionalized, ambulatory, community-living adults) | >=130 (SBP) | <130 (SBP) |
specific comorbidities |
|
|
diabetes | >=130/80 | <130/80 |
chronic kidney disease | >=130/80 | <130/80 |
chronic kidney disease post-renal transplant | >=130/80 | <130/80 |
heart failure | >=130/80 | <130/80 |
stable ischemic heart disease | >=130/80 | <130/80 |
secondary stroke prevention | >=140/90 | <130/80 |
peripheral arterial disease | >=130/80 | <130/80 |
|
|
|
How effective is blood pressure lowering in reducing the risk of future cardiovascular events?
Effects of lowering blood pressure:
- in a large-scale analysis of randomised trials (4)
- a 5 mm Hg reduction of systolic blood pressure reduced the risk of major cardiovascular events (defined as a composite of fatal and non-fatal stroke, fatal or non-fatal myocardial infarction or ischaemic heart disease, or heart failure causing death or requiring admission to hospital) by about 10%, irrespective of previous diagnoses of cardiovascular disease, and even at normal or high-normal blood pressure values
- hazard ratios (HR) associated with a reduction of systolic blood pressure by 5 mm Hg for a major cardiovascular event
- in participants without previous cardiovascular disease was 0.91, 95% CI 0.89-0.94
- in partipants with previous cardiovascular disease was 0.89, 0.86-0.92
- findings suggest that a fixed degree of pharmacological blood pressure lowering is similarly effective for primary and secondary prevention of major cardiovascular disease, even at blood pressure levels currently not considered for treatment
- a 5 mm Hg reduction of systolic blood pressure reduced the risk of major cardiovascular events (defined as a composite of fatal and non-fatal stroke, fatal or non-fatal myocardial infarction or ischaemic heart disease, or heart failure causing death or requiring admission to hospital) by about 10%, irrespective of previous diagnoses of cardiovascular disease, and even at normal or high-normal blood pressure values
What should be the blood pressure target if increased cardiovascular risk (5)
- the SPRINT Research Group noted that among patients who were at increased cardiovascular risk
- targeting a systolic blood pressure of less than 120 mm Hg resulted in lower rates of major adverse cardiovascular events and lower all-cause mortality than targeting a systolic blood pressure of less than 140 mm Hg, both during receipt of the randomly assigned therapy and after the trial
- used a fully automated oscillometric BP monitor to document BP measurements
- rates of some adverse events were higher in the intensive-treatment group
- targeting a systolic blood pressure of less than 120 mm Hg resulted in lower rates of major adverse cardiovascular events and lower all-cause mortality than targeting a systolic blood pressure of less than 140 mm Hg, both during receipt of the randomly assigned therapy and after the trial
Reference:
- NICE (August 2019). Clinical management of primary hypertension in adults
- NICE (April 2022). Stroke and transient ischaemic attack in over 16s: diagnosis and initial management
- Whelton PK et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018;138(17):e426-e483.
- The Blood Pressure Lowering Treatment Trialists' Collaboration. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet 2021; 397: 1625-36.
- The SPRINT Research Group. Final Report of a Trial of Intensive versus Standard Blood-Pressure Control.N Engl J Med 2021; 384:1921-1930
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.