Assessment of vaginal discharge
Various aspects of the history may be suggestive of particular infectious causes of an increased vaginal discharge;
- pregnancy, diabetes mellitus, recent antibiotic treatment, immunosuppression, dyspareunia or itchy vulval irritation - suggestive of candidiasis (1)
- a recent change in sexual partner, a discharge that is offensive and copious - suggestive of trichomoniasis (2)
- offensive discharge plus IUCD plus dyspareunia - suggestive of bacterial vaginosis (3)
- erythema and oedema of the vulvovaginal area, excoriation of the vulva and presence of curd-like discharge with white plaques - suggestive of candidiasis
- yellow/green, offensive, frothy discharge - suggestive of trichonomiasis
- bacterial vaginosis is suggested by a thin, offensive, grey-white, adherent discharge
Management of Women Presenting with Vaginal Discharge outside the Genitourinary Medicine Clinic Setting (4)
- Clinical and sexual history
- when a woman presents with a vaginal discharge that she feels is different from her normal discharge this should be assessed by first taking a clinical history
- she may have underlying concerns (e.g. STI or cancer) or specific expectations that should be explored
- the presence of vaginal discharge is, in itself, a poor predictor of an STI
- nevertheless, a sexual history (e.g. number and gender of partners, sexual activities, use of condoms) should be taken to assess the risk of STIs
- sexually active women are at higher risk of STI if they are
- aged <25 years; or
- have changed their sexual partner or
- had more than one sexual partner in the last 12 months
- sexually active women are at higher risk of STI if they are
- other risk factors include a lack of consistent condom use, and a previous diagnosis of chlamydia infection in the last 12 months
- nevertheless, a sexual history (e.g. number and gender of partners, sexual activities, use of condoms) should be taken to assess the risk of STIs
- when a woman presents with a vaginal discharge that she feels is different from her normal discharge this should be assessed by first taking a clinical history
Assessment of symptoms
- symptoms associated with vaginal discharge can guide a health professional to the most likely cause
Sign/Symptom | Bacterial Vaginosis | Candida | Trichomoniasis |
Discharge | Thin | Thin White | Scanty to profuse |
Odour | Offensive/fishy | Non-offensive | Offensive |
Itch | none | vulval itch | vulval itch |
Other possible symptoms | Soreness; Dysuria;Superficial dyspareunia | Dysuria; lower abdominal pain | |
Visible signs | Discharge coating the vagina and vestibule; No vulval inflammation | Normal findings OR Vulval erythema; Oedema; fissuring; satellite lesions | Frothy yellow discharge; vulvitis; vaginitis; cervicitis; 'Strawberry cervix' (ectocervix sometimes resembles the surface of a strawberry) |
Point-of-care test: vaginal pH | > 4.5 pH | <= 4.5 | >4.5 |
- the characteristics of the vaginal discharge should be determined:
- what has changed
- onset
- duration
- odour
- cyclical changes
- colour
- consistency
- exacerbating factors (e.g. after intercourse)
- enquiry should also cover any associated symptoms:
- itching
- superficial dyspareunia
- vulval or vaginal pain
- dysuria
- abnormal bleeding (heavy, intermenstrual or post-coital)
- deep dyspareunia
- pelvic or abdominal pain
- fever
Examination, point-of-care investigations and STI testing
- history-taking alone may guide health professionals towards the most likely diagnosis but diagnostic accuracy varies
- in addition to the clinical and sexual history, physical examination and vaginal pH may be helpful
- should be standard clinical practice to offer to examine people presenting with genital symptoms
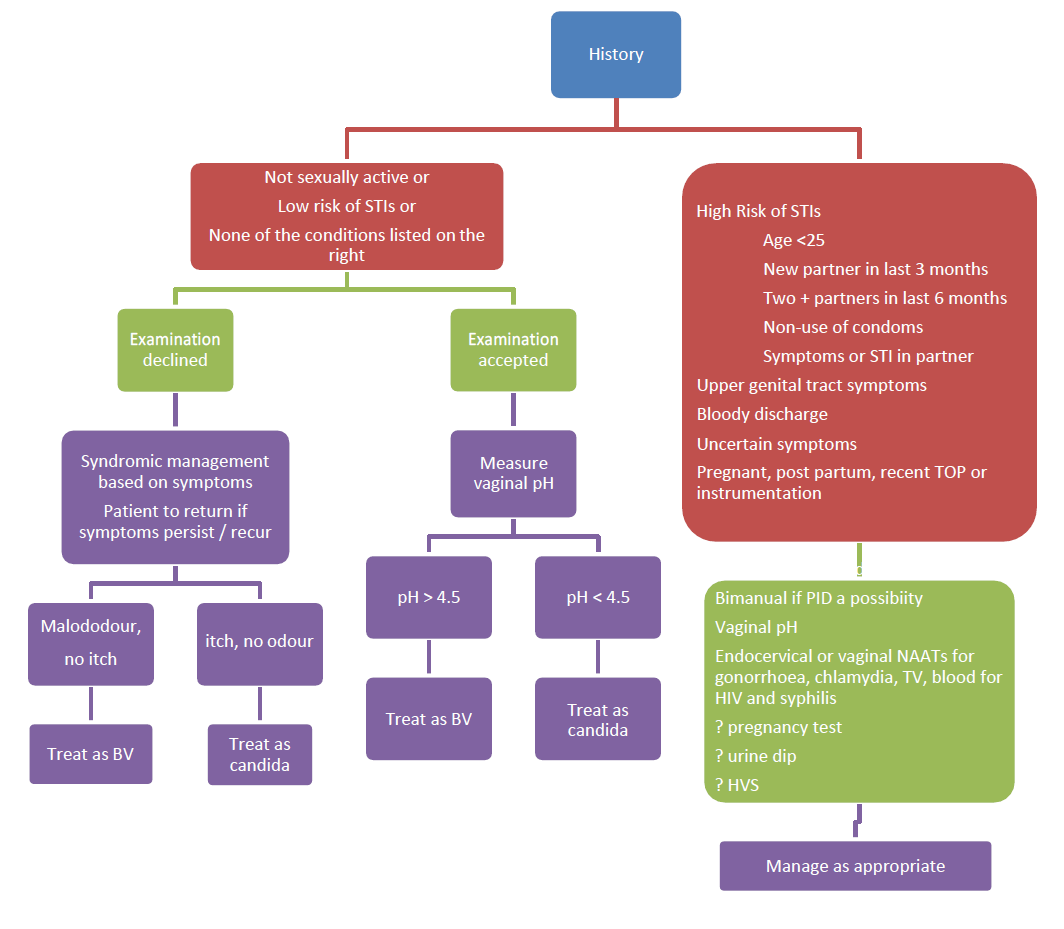
- however if the history indicates candidiasis or BV, the risk of STI is low, and there are no symptoms indicative of upper genital tract infection, treatment for candidiasis or BV may be given without examination (i.e. syndromic management) Schemata for diagnosis of Candida, BV and TV by signs and symptoms in adult women (5)
- women should be advised to undergo examination if symptoms persist or reoccur
- women should be advised to undergo examination if symptoms persist or reoccur
- however if the history indicates candidiasis or BV, the risk of STI is low, and there are no symptoms indicative of upper genital tract infection, treatment for candidiasis or BV may be given without examination (i.e. syndromic management) Schemata for diagnosis of Candida, BV and TV by signs and symptoms in adult women (5)
- STI testing should ideally be offered to all sexually active women
- for women who decline an offer of examination, a self-taken vulvovaginal swab (VVS) may be an option for chlamydia +/-gonorrhoea testing by nucleic acid amplification test (NAAT)
- urine tests are appropriate for men but in women NAAT testing of VVS or endocervical swabs are preferable to urine
- women who accept examination should have a vaginal pH measurement using narrow range pH paper (pH 4-7)
- secretions should be collected from the lateral sides of the vaginal wall using a loop or swab. Vaginal pH testing can be used to assess the likelihood of candida (pH<= 4.5) or of BV or TV (pH >4.5) but it cannot distinguish between BV and TV
- if STI testing is indicated and/or requested, endocervical swabs for chlamydia and gonorrhoea should also be taken, and a high vaginal swab (HVS) may be indicated in some cases
- physical examination should include:
- inspection of the vulva (for obvious discharge, vulvitis, ulcers, other lesions or changes)
- speculum examination (inspection of: vaginal walls, cervix, foreign bodies; amount, consistency and colour of discharge)
- where there is any suggestion of upper genital tract infection physical examination should also include:
- abdominal palpation (for tenderness/mass)
- bimanual pelvic examination (adnexal and/or uterine tenderness/mass, cervical motion tenderness)
- there is agreement in the UK that the minimum tests that constitute an STI screen are chlamydia, gonorrhoea, syphilis and HIV tests
- lengthy pre-test discussion is not required unless a patient needs or requests this
- HIV testing in primary care settings has been encouraged by Chief Medical and Nursing Officers
References:
- Centers for Disease Control and Prevention. Vaginal candidiasis. Oct 2021 [internet publication].
- Schumann J. Trichomoniasis. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan.2023 Jun 12.
- Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. 2021 Jul 23;70(4):1-187.
- FSRH and BASHH Guidance (February 2012) Management of Vaginal Discharge in Non-Genitourinary Medicine Settings.
- Oxfordshire Clinical Commissioning Group. Investigation and Management of Vaginal Discharge in Adult Women
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.