Relationship between PSA and prostate cancer
- the value of PSA testing in asymptomatic men is unclear
- estimates suggest that, using a PSA screening cut-off concentration of 4ng/mL or more, 13% of men with cancer will be missed but go on to present with the cancer in the next 4 years
- of the men identified with cancer by screening, a proportion will never develop clinically significant disease
- the PSA test does not clearly differentiate men who do and do not have prostate cancer
- in a study involving 300 symptomatic men aged at least 50 years, prostate biopsy revealed cancers in around 11% of those with a PSA concentration of up to 4ng/mL, in around 26% with a concentration of 4.1-10ng/mL, and in around 64% with a concentration of 10ng/mL or more (2,3)
- however the study did provide evidence that a combination of measurement of the serum PSA concentration and rectal examination, with ultrasonography performed in patients with abnormal findings, provides a better method of detecting prostate cancer than rectal examination alone
- estimates suggest that, using a PSA screening cut-off concentration of 4ng/mL or more, 13% of men with cancer will be missed but go on to present with the cancer in the next 4 years
- a more recent review states (4):
- PSA aims to detect localised prostate cancer when treatment can be offered that may cure cancer or extend life. It is not usually recommended for asymptomatic men with less than 10 years life expectancy
- evidence suggests PSA screening could reduce prostate-cancer related mortality by 21%
- about 3 in 4 men with a raised PSA level (>=3ng/ml) will not have cancer. The PSA test can also miss about 15% of cancers
- Before a PSA test men should not have:
- an active urinary infection
- ejaculated in previous 48 hours
- exercised vigorously in previous 48 hours
- had a prostate biopsy in previous 6 weeks
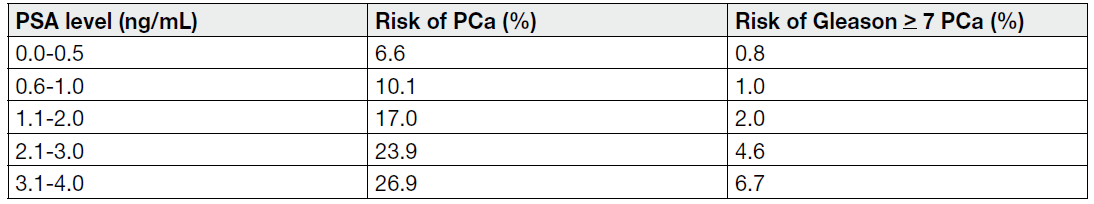
- PSA is a continuous parameter, with higher levels indicating greater likelihood of prostate cancer. Many men may harbour prostate cancer despite having low serum PSA The table demonstrates the occurrence of Gleason > 7 prostate cancer at low PSA levels, precluding an optimal PSA threshold for detecting non-palpable but clinically significant prostate cancer Risk of Prostate Cancer in relation to low PSA values (5)
There is a strong association between baseline prostate specific antigen (PSA) and prostate cancer mortality (6):
- evidence suggests that 44% of prostate cancer deaths occur in men with PSA in the top 10% of the PSA distribution at ages 44–49 year
- only 0.2% of men with PSA below 1.0 ng/mL at age 60 years died from prostate cancer within 25 years
A study found that the 5-year incidence of aggressive prostate cancer was low for men with PSA levels of 1 ng/mL or less (7)
- 10-year incidence of aggressive disease was also low for men aged 65 or older with PSA levels of 0.5 ng/mL or less
A study investigated the subsequent prevalence of prostate cancer in a group with PSA <= 4.0 ng/ml (8):
- during a seven-year period, none of the men in this analysis had PSA levels above 4.0 ng per milliliter or any abnormality on digital rectal examination
- all participants underwent a prostate biopsy at the end of the study
- of almost 3000 men in the group, 15 percent had a prostate cancer on the end-of-study biopsy, and of these cancers, 15 percent were high grade (a Gleason score of 7 to 9)
- prevalence of cancer increased with the PSA level, from 7 percent among men with PSA values of 0.5 ng per milliliter or less to 27 percent among men with PSA values of 3.1 to 4.0 ng per milliliter
- prevalence of high-grade disease also increased with the PSA level, from 13 percent when the PSA level was 0.5 ng per milliliter or less to 25 percent when the PSA level was 3.1 to 4.0 ng per milliliter
In high-grade prostate cancer a low or a high PSA predicts poor outcome (9):
- in a large dataset describing the prognostic value of prostate-specific antigen (PSA) in localised prostate cancer
- in high-grade prostate cancer, a low or high PSA predicts poor outcomes
- in low/intermediate-grade prostate cancer, the higher the PSA the worse the outcome
- confirms a more aggressive biology in low PSA secreting high-grade prostate cancer
Reference:
- Drug and Therapeutics Bulletin (2004); 42(11):81-5.
- Catalona WJ et al. Measurement of prostate-specific antigen in serum as a screening test for prostate cancer. N Engl J Med 1991; 324: 1156-61.
- Corrections. N Engl J Med 1991; 325: 1324.
- PHE (2016). Advising well men aged 50 and over about the PSA test for prostate cancer: information for GPs
- European Association of Urology 2018. Guidelines on Prostate Cancer
- Heijnsdijk EAM et al. Lifetime Benefits and Harms of Prostate-Specific Antigen-Based Risk-Stratified Screening for Prostate Cancer. J Natl Cancer Inst. 2020 Oct 1;112(10):1013-1020.
- Landy R et al. Risk of Prostate Cancer-related Death Following a Low PSA Level in the PLCO Trial. Cancer Prev Res (Phila). 2020 Apr;13(4):367-376.
- Thompson IM, Pauler DK, Goodman PJ, et al. Prevalence of prostate cancer among men with a prostate-specific antigen level of ≤4. 0 ng per milliliter. N Engl J Med. 2004;350:2239–46.
- Fankhauser CD et al. A low prostate specific antigen predicts a worse outcome in high but not in low/intermediate-grade prostate cancer. Eur J Cancer. 2023 Mar;181:70-78.
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page