Chronic renal failure is the progressive loss of nephrons resulting in permanent compromise of renal function.
The classification of chronic kidney disease (CKD) is based on estimated GFR, and recognises five stages of kidney disease, as follows (1,2):
- Stage 1: Normal GFR; GFR >90 mL/min/1.73 m2 with other evidence of chronic kidney damage
- Stage 2: Mild impairment; GFR 60-89 mL/min/1.73 m2 with other evidence of chronic kidney damage
- Stage 3: Moderate impairment; GFR 30-59 mL/min/1.73 m2
- Stage 3 CKD should be split into two subcategories defined by (2):
- GFR 45-59 ml/min/1.73 m2 (stage 3A)
- GFR 30-44 ml/min/1.73 m2 (stage 3B)
- Stage 3 CKD should be split into two subcategories defined by (2):
- Stage 4: Severe impairment: GFR 15-29 mL/min/1.73 m2
- Stage 5: Established renal failure (ERF): GFR < 15 mL/min/1.73 m2 or on dialysis (the term established renal failure is used instead of end-stage renal disease or end-stage renal failure, as this is the term used in the National Service Framework for Renal Services)
- other evidence of chronic kidney damage may be one of the following:
- persistent microalbuminuria
- persistent proteinuria
- persistent haematuria (after exclusion of other causes, e.g. urological disease)
- structural abnormalities of the kidneys demonstrated on ultrasound scanning or other radiological tests, e.g. polycystic kidney disease, reflux nephropathy
- biopsy-proven chronic glomerulonephritis (most of these patients will have microalbumuria or proteinuria, and/or haematuria)
- patients found to have a GFR of 60-89 mL/min/1.73 m2 without one of these markers should not be considered to have CKD and should not be subjected to further investigation unless there are additional reasons to do so (1)
CKD is defined as persistent abnormalities in kidney structure or function for more than three months, manifest as either low GFR or presence of a marker of kidney damage (3)
NICE suggest (2):
- clinicians should use urine albumin:creatinine ratio (ACR) in preference to protein:creatinine ratio (PCR) in order to detect proteinuria
- ACR has greater sensitivity than protein:creatinine ratio (PCR) for low levels of proteinuria. For quantification and monitoring of proteinuria, PCR can be used as an alternative. ACR is the recommended method for people with diabetes
- for the initial detection of proteinuria, if the ACR is between 3 mg/mmol and 70 mg/mmol, this should be confirmed by a subsequent early morning sample. If the initial ACR is 70 mg/mmol or more, a repeat sample need not be tested
- regard a confirmed ACR of 3 mg/mmol or more as clinically important proteinuria
- quantify urinary albumin or urinary protein loss for:
- people with diabetes
- people without diabetes with a GFR of less than 60 ml/min/1.73 m^2
- NICE suggested a classification of CKD incorporating GFR and ACR (2)
ACR (albumin creatinine ratio) category | ACR (mg/mmol) |
A1 | <3 |
A2 | 3-30* |
A3 | >30** |
- * Relative to young adult level
- ** Including nephrotic syndrome (ACR usually >220 mg/mmol)s
- CKD is classified according to estimated GFR (eGFR) and albumin:creatinine ratio (ACR), using 'G' to denote the GFR category (G1-G5, which have the same GFR thresholds as the CKD stages 1-5 recommended previously) and 'A' for the ACR category (A1-A3), for example:
- a person with an eGFR of 25 ml/min/1.73 m2 and an ACR of 15 mg/mmol has CKD G4A2.
- a person with an eGFR of 50 ml/min/1.73 m2 and an ACR of 35 mg/mmol has CKD G3aA3
- an eGFR of less than 15 ml/min/1.73 m2 (GFR category G5) is referred to as kidney failure
- it is noted that:
- increased ACR is associated with increased risk of adverse outcomes
- decreased GFR is associated with increased risk of adverse outcomes
- increased ACR and decreased GFR in combination multiply the risk of adverse outcomes
This is summarised as (4):
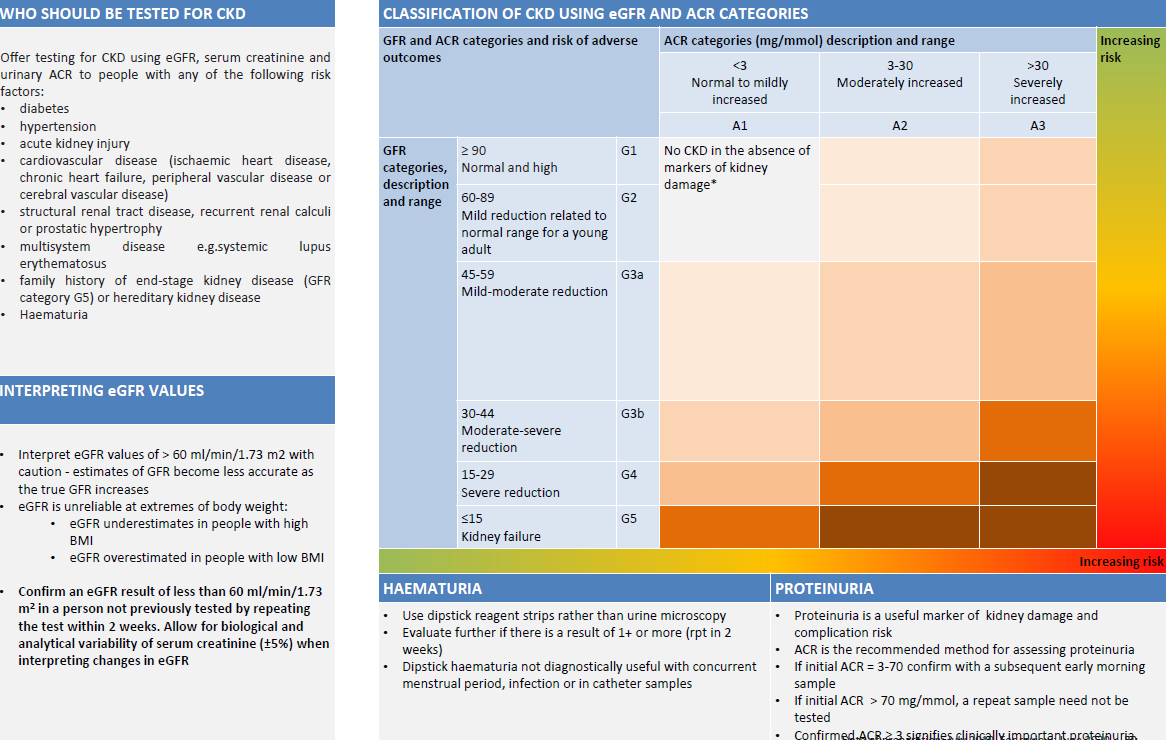
Abbreviations: ACR, albumin:creatinine ratio; CKD, chronic kidney disease
Notes:
- consider using eGFRcystatinC at initial diagnosis to confirm or rule out CKD in people with:
- an eGFRcreatinine of 45-59 ml/min/1.73 m2, sustained for at least 90 days and
- no proteinuria (albumin:creatinine ratio [ACR] less than 3 mg/mmol) or other marker of kidney disease
- do not diagnose CKD in people with:
- an eGFRcreatinine of 45-59 ml/min/1.73 m2 and
- an eGFRcystatinC of more than 60 ml/min/1.73 m2 and
- no other marker of kidney disease
- use of renin-angiotensin system antagonist to people with CKD based on ACR:
- angiotensin-converting enzyme inhibitors (ACE inhibitors)/ angiotensin-II receptor blockers (ARBs) should be offered to non-diabetic people with CKD:
- diabetes and an ACR of 3 mg/mmol or more (ACR category A2 or A3)
- hypertension and an ACR of 30 mg/mmol or more (ACR category A3)
- an ACR of 70 mg/mmol or more (irrespective of hypertension or cardiovascular disease)
- angiotensin-converting enzyme inhibitors (ACE inhibitors)/ angiotensin-II receptor blockers (ARBs) should be offered to non-diabetic people with CKD:
Reference:
- (1) The Renal Association (May 2006).UK CKD Guidelines.
- (2) NICE (August 2021). Chronic kidney disease: assessment and management
- (3) Chen T K, Hoenig M P, Nitsch D, Grams M E. Advances in the management of chronic kidney disease. BMJ 2023; 383 :e074216 doi:10.1136/bmj-2022-074216
- (4) The North West London Health and Care Partnership. North West London Diabetes Guidelines (Accessed 30/6/2020).
Related pages
- Staging of chronic kidney disease (CKD)
- Aetiology
- History
- Clinical features of chronic renal failure
- Early identification of CKD in primary care
- Diagnosis and investigations in renal failure
- Management
- Complications
- Prognosis
- Referral criteria from primary care - kidney disease
- Monitoring of chronic kidney disease (CKD)
- Deteriorating eGFR in CKD
- Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) creatinine equation to estimate GFR (eGFR)
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page